Having a child can be a life changing and enriching experience, and having the right healthcare provider by your side can be an extremely important source of support and information. An Obstetrician is a doctor that specialises in providing medical care and advice before, during and after birth, to ensure that you experience a smooth, […]
Dr Rahul Sen | Specialist care for birth and beyond | Sydney, Australia
Clinic conveniently located in Edgecliff : Freecall 1800 890 964
Blog
5 tips for selecting the right obstetrician for you
Pregnancy can be an incredibly emotional and turbulent time for women and their families, so having the right medical partner by your side is vital to a happy, healthy nine months. An obstetrician is a doctor who specialises in providing advice and medical care throughout, during and after your pregnancy. They are there for every […]
Preparation For Birth
As we approach your due date I like to have a longer discussion with you and your partner, to discuss your birth plan. You do not need to have a written document, it is good to be informed, and to have an idea of how you would like the birth to go, but it is […]

Long-haul Flight Advice
Issues: Radiation: you are exposed to a small increase in the amount of exposure to background radiation Security: consider not only the customs and safety of the country you are visiting, but remember motor vehicle accidents are a leading cause of travel injury Water: drink only safe, bottled water Food: eat freshly and properly cooked […]

Supplements you might be prescribed in pregnancy
This month I thought we’d focus on some other common supplements you may be prescribed in pregnancy. Vitamin D Many pregnant women have reduced vitamin D levels. You are at increased risk of deficiency if you have dark skin or are veiled, but also if you use sunscreen regularly or spend little time outdoors. It […]

Eat out safely when you are pregnant – Pregnancy diet plan
Between nausea, the worry about listeria and the need to ensure a high-quality diet lunchtime choices can be difficult! If you usually bring your lunch to work it is likely you will need to make some changes from your usual options- but is what you are choosing now a healthy option? Hot chips may be […]

Leg cramps during pregnancy: causes and treatment.
It’s quite common to experience leg cramps during pregnancy, particularly in the third trimester. Nearly half of all pregnant women suffer from muscle spasms in their legs, with cramping more frequent during the evening. What causes leg cramps during pregnancy? Leg cramps may be caused by the additional weight gain of pregnancy and changes in […]
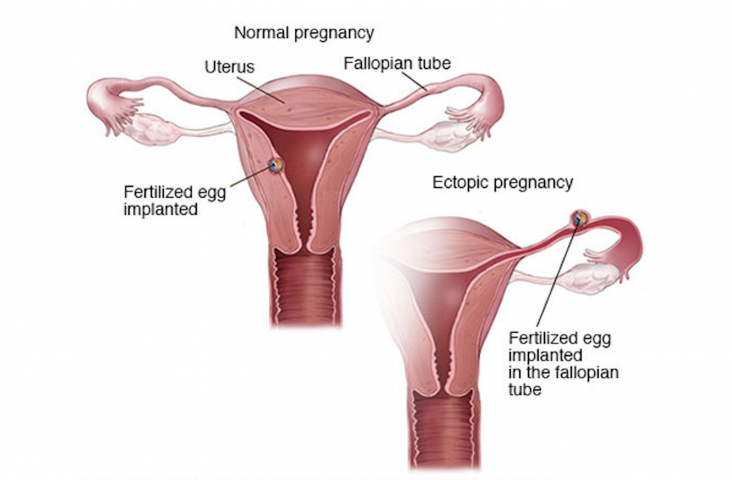
Ectopic pregnancy – treatment overview.
In most cases, an ectopic pregnancy is treated right away to avoid rupture and severe blood loss. The decision about which treatment to use depends on how early the pregnancy is detected and women’s overall condition. For an early ectopic pregnancy that is not causing bleeding, you may have a choice between using medicine or […]

Pregnancy Planning – Maternity Leave
If you are planning a pregnancy in the nearest future, it is important to think about your maternity leave. Sometimes a few months could be the difference between whether or not you’re entitled to take leave or whether you are eligible for a maternity leave payment. That’s why in today’s article we would like to […]

Pregnancy nutrition – Eating seafood
Unless you are vegetarian, it’s ideal to have seafood feature in your diet regularly! This may include white fish, pink/oily fish and shellfish such as prawns, lobster, bugs as well as scallops and mussels. Seafood gives you a valuable source of protein, B vitamins, iron, zinc and especially iodine and omega-3 fatty acids. The iodine […]