During Pregnancy (Antenatal)
Information on Pregnancy Care 2025
Congratulations on your pregnancy and welcome!
Thank you for choosing me as your obstetrician. As a father myself I know this is a truly special time in your life. I have written this as a guide to what you can expect from your pregnancy care. Of course, I look forward to discussing the important issues with you in person, as well as addressing any specific questions or concerns you may have.
My philosophy is “Your body, your baby, your choice”. My aim is to help you do it your way and to make your pregnancy journey a safe, happy and enjoyable experience.
My team and I look forward to taking care of you.
I usually like to see you at 8 weeks for a dating scan, which I do in my rooms. Please come with a “comfortably” full bladder for the scan.
If you have conceived through IVF then they will usually have arranged a scan at 7 weeks for you. In that case please come and see me at 9 weeks for a progress scan. If you wish to do genetic carrier screening then please do this before you see me. The triple screen for cystic fibrosis, spinal muscular atrophy and fragile X is now covered my Medicare. I can send you a referral form. The result takes 3-4 weeks, so it should be done as soon as possible.
These are the things I need for your first visit:
• Referral from your GP (if you want to claim a Medicare rebate
• Summary of your medical history, medications and allergies, if not listed in the letter from your GP
• Antenatal booking blood tests: I can send the form to you if your GP has not done them
• Copies of any pregnancy ultrasound scans you have had
• Details of your most recent cervical screening (Pap) test
Your first visit usually takes 50-55 minutes.
Dr Rahul Sen
Obstetric Care
Your Pregnancy Timeline:
4 weeks: First missed menstrual period (around 2 weeks from actual conception)
8 weeks: Dating ultrasound, usually in my rooms – you will need a “comfortably full” bladder. Referral for antenatal booking blood tests if not already done by your family doctor. Antenatal visits now every 4-5 weeks (1st baby) or 5-6 weeks (2nd + baby)
10-11 weeks: Blood tests for the Nuchal Translucency Scan (if you are having one)
11 weeks: Earliest time for Non-Invasive Prenatal Test (Harmony, Panorama or Generation 46)
12-13 weeks: Early Structural Scan or Nuchal Translucency Scan (if you are having one). Book in for antenatal classes (and maybe Calmbirth,) if booked at RHW
14-20 weeks: Submit Hospital booking form – paper form for RHW, online booking for POWPH
18-24 weeks: Appointment to see midwife Bridget (or Orla) for first consultation (F2F or Zoom)
20-21 weeks: Detailed morphology ultrasound scan. Can be earlier but later images are better. Start feeling baby’s movements (sometimes later if the placenta is at the front)
20-24 weeks: Book in for antenatal classes, if booked at POWPH (first baby)
26-28 weeks: Gestational diabetes screen (Overnight fast. 3 blood tests. Allow 3 hours. Must book.)
28-30 weeks: Anti D injection, if your blood group is Rhesus negative (unless partner also Rh Neg)
Antenatal visits now every 2 weeks (1st baby) or every 3 weeks (2nd + baby)
30-33 weeks: 3D ultrasound: “fun” scan to see baby’s face. On a Saturday in Edgecliff rooms
34-36 weeks: Second Anti D injection, if required.
36-37 weeks: Growth and wellbeing ultrasound. Book at Ultrasound Care, like 20 week scan. Vaginal-perianal swab for Group B Streptococcus (GBS) if planning vaginal birth. Antenatal visits now weekly (all pregnancies). Second, consultation with Bridget (or Orla), if required (F2F or Zoom)
34-37 weeks: Start discussing birth plan. Sign consent for elective/emergency caesarean
39-40 weeks: Usual timing of elective caesarean section if you want or need one
39-41 weeks: Usual timing of induction of labour if you want or need one
40 weeks: Full term
3D scans are best performed at 30-33 weeks in Edgecliff
Please note that your medical information is confidential, and I do not discuss your details with anyone
other than health staff and professionals who are involved in your care.
NB. I never discuss results or medical care by phone, but I can see you urgently if needed.
Choice of Hospitals
I usually prefer Prince of Wales Private Hospital over Royal Hospital for Women. Both are good hospitals, and the birth suite midwives are generally excellent. I hope the following information helps.
Advantages of Royal Hospital for Women
• An on-site neonatal intensive care unit if you have a very pre-term baby (eg twins)
• More cost effective if you do not have private health insurance or do not have obstetric cover
• Option for early discharge on the Midwifery Support Programme (MSP), where midwives visit you at home if you leave hospital early, and if you live in the catchment area
Disadvantages of Royal Hospital for Women
• You will be in a shared room unless your health insurance specifies single room cover
• I cannot choose my own anaesthetist for your caesarean or epidural if you want one
• Stricter hospital protocols, which allows less flexibility and autonomy. For example, we may decide
jointly that we wish to induce labour, but the request can be over-ruled by the hospital protocols
• The hospital is less supportive of elective caesarean section on request, and is generally less well
geared towards private patients.
• Not all ward services are provided by consultants: eg the pre-admission clinic and some ward
rounds are done by registrars and the pain team, rather than by your anaesthetist.
• The Hospital is getting old, and the rooms are in need of refurbishment.
• The food is not as good, and meals are served in a communal area, and not brought to you.
• You need to bring more of your own things, such as nappies and baby wipes
Advantages of Prince of Wales Private Hospital
• There are only private rooms in maternity
• The hospital has just been refurbished, is more modern and has nicer rooms and better meals.
• The hospital is geared towards private patients with specialist led care and less regulatory hurdles.
• It is easier to see a lactation consultant
Disadvantages of Prince of Wales Private Hospital
• Once you leave the hospital it can be more difficult to be readmitted if there are any complications.
• The rooms are not all the same size
NB. There is no longer a night nursery, nor Little Luxuries programme at the Crowne Plaza.
In reality both hospitals are good and safe, and the differences between them are relatively small.
Many women struggle with breast feeding and often get conflicting advice. This is common in all
maternity hospitals. My midwifery team tries to provide good support, after discharge from hospital.
Both hospitals have some restrictions in relation to infection risk including limiting visitors
What to do in an Emergency:
If you ever have severe pain, very heavy bleeding, shortness of breath or chest pain the safest
thing to do is call an ambulance to take you to the nearest emergency department.
Under 20 Weeks:
Please contact my rooms as soon as possible. I have emergency appointments most weekdays, and
can usually arrange to see you the same day and perform an ultrasound scan in rooms.
20 weeks and over:
Please contact the delivery suite of the hospital at which you are booked:
Prince of Wales Private Hospital: 9650 4444
Royal Hospital for Women: Triage Number: 0439 869 035 or 9382 6100
Baby Emergencies:
I strongly recommend that you learn Baby and Child CPR and First Aid with a 6 hour course:
Website: www.cprkids.com.au or email: hello@cprkids.com.au or Tel: 1300 543 727
Sydney Children’s Hospital also provides excellent emergency care for babies.
Emergency First Aid for Baby: www.littlelives.com.au
Vaginal Birth or Caesarean Section?
Some women know exactly what they want from birth, in which case I will do my best to make that
happen in a safe and enjoyable way. This summary is for women who want to know a bit more about
the pros and cons of vaginal birth and caesarean section for both mother and baby, so that you can
make a fully informed decision regarding your preference.
Vaginal birth is, of course, the traditional way of giving birth and women throughout the ages have
given birth, with excellent outcomes for both mother and baby. There are, however, both risks and
benefits of planned vaginal birth, as there are for planned caesarean section.
In general things are more controlled and predictable with planned caesarean section than with
planned vaginal birth. One thing to bear in mind is that whatever is planned is that whatever you are
planning things can change. With planned caesarean section you may go into labour prior to the
planned caesarean date or we may need to bring forward the timing of birth.
With planned vaginal birth there is greater unpredictability regarding timing of birth and birth outcomes.
With regard to timing most women in their first pregnancy will labour at 3-4 days after their due date.
You have the option of being induced any time from 39 weeks onwards.
In terms of outcomes women in their first labour statistically have the following outcomes: 20% chance
of emergency caesarean section, 15% chance of vacuum (ventouse) delivery and 5-10% chance of
forceps delivery. Around 30-40% of women will need an episiotomy (cut with scissors). 80-90% of
women will need stitches, that mostly heal very well. Around 3-4% of women will have a 3rd or 4th
degree perineal tear and around 20% will have some pelvic floor injury, resulting in poorer bladder
control. 3rd and 4th degree tears can also result in reduced control of bowel motions, fluid or gas.
Ultimately I believe in your choice to determine your own plan for birth. For women who want particular
timing you can still have a planned induction of labour. In relation to timing, it is generally not
recommended to plan delivery before 39 weeks, whether you are planning a vaginal birth or caesarean.
Advantages of planned Vaginal Birth for Mother
• Generally a quicker recovery, especially if the birth is uncomplicated
• The benefits are increased the more births you have: in general vaginal births become quicker and easier the more you have whereas caesareans can become slightly harder and riskier
• You reduce the risk of placenta praevia, where the placenta is in the way of the birth canal, and placenta accreta, where the placenta is abnormally adherent and can cause haemorrhage.
Advantages of planned Caesarean Birth for Mother
• This avoids some of the uncertainty regarding planned vaginal birth, such as timing of birth, emergency caesarean section, vacuum and forceps birth
Advantages of planned Vaginal Birth for Baby
• More of the fluid is squeezed out of the baby’s lungs coming through the birth canal, which means reduced rates of transient tachypnoea of the newborn (TTN)
• The baby picks up “good” bacteria coming through the birth canal and those bacteria populate their gut and entire body (microbiome). This appears to have advantages for gut health and reduced immune and autoimmune diseases
• Vaginal birth may promote better lactation and breast feeding
Advantages of planned Caesarean Section for Baby
• This avoids fetal distress in labour, and the rare but serious complication of hypoxic ischaemic encephalopathy
• This avoids birth related trauma, including injury from forceps or vacuum, such as skull fracture, bleeding in the brain or under the scalp or injury to the nerves of the face.
My Team:
Secretaries: Peta Bellanto, Nathalie Moutou
Midwife: Bridget Flannery, supported by Michele Simpson and Orla Priestley
My background
I grew up in the UK but have lived in Australia for over 40 years. I began my medical training at the University of Sydney, Royal Prince Alfred Hospital, The Canberra Hospital and the Royal Hospital for Women, where I completed my core obstetric training. I then worked at Queen Charlotte’s & Chelsea Hospital in London, where I completed my advanced training and gained extra consultant experience, especially in diabetes and high-risk obstetrics, before returning to Sydney as a specialist.
I am experienced in both uncomplicated and high-risk obstetrics, as well as the care of pregnant women with medical disorders, such as diabetes and recurrent miscarriage. I am currently involved in the training, supervision and examination of junior doctors. I enjoy teaching obstetric emergencies and introduced the Managing Obstetric Emergencies and Trauma (MOET) into Australia from the UK in 2009. I am an expert witness for medico-legal cases and have just completed a Masters of Health Law.
Introducing my Midwife:
I am both fortunate and delighted to have Bridget Flannery as my midwife. Bridget is an experienced and skilled midwife, with whom I have worked for many years at POWPH, where she was midwife in charge. She will see you (first baby) for a first consultation at 18-24 weeks, and then for a second consultation at 36 weeks, if needed. Her colleague, Orla Priestley, will provide back-up cover for, nwhere needed. Appointments are generally in person in Edgecliff, but can be via Zoom if preferred.
Bridget is not present for the birth, however she follow you up post natally. Please text Bridget when you leave hospital and, where possible, she will do one postnatal consultation, as well as provide some text message and phone support. If you need more help than Briget can provide with a single visit she will put you in touch with someone who can provide more extensive assistance. Bridget has a special interest in perinatal mental health, and as part of her antenatal sessions with you she will spend some time with both you and your partner together, and also with you on your own.
Bridget is a qualified lactation consultant. She is an excellent point of contact if you have additional general or midwifery questions between your visits with me. She can be contacted by text message, between the hours of 9am and 9pm most days, and occasionally by phone. Please note that Bridget has a busy public hospital schedule, and is a wife and mother, in addition to her work with my practice. For that reason she is not contactable on some days, overnight or some weekends.
Please note that Bridget is not the person to contact for emergencies: please contact the delivery suite of the hospital at which you are booked, whether before or after the birth.
The cost of Bridget’s care and advice is incorporated in your planning and management fee.
Message from Bridget Flannery
Hello, I'm Bridget an Endorsed Registered Midwife and Registered Nurse. I have been working with women, babies and their families for nearly 20 years.
I believe pregnancy and birth in not just about bringing babies into the world, but about journeying with women to become mothers and educating their family and friends about how they can best support them.
As part of Dr Sen's midwifery team, I am here to help you plan for the arrival of your baby and provide you with midwifery care, education, lactation and feeding support throughout the postnatal period.
Midwifery Cover
If Bridget is unavailable I have other great midwives who will help, including Michele Simpson, Orla Priestley and Chantelle Du Boisee.
Counselling and Psychological Support
Psychologists:
Cloudberry Clinic: A clinical psychology practice located in Randwick. We are allies in your transition to motherhood. We deliver care and evidence-based treatments for women's mental health concerns, perinatal psychology and mentoring for life and career. Services across the antenatal and postnatal period include but are not limited to support for anxiety, depression, stress, fertility issues, birth debriefing, adjustment to mothering, relationship stress, parenting challenges, work pressures, medical complications, grief and loss.
Dr Wendy Roncolato, Sophie Lynn-Evans, Daisy Prowse, Emily Arkell, Brooke Jericho, Mia Birkner and Dr Megan Jeon
42a Frenchman’s Rd, Randwick.
Tel: 1300 553 722
Web: www.cloudberryclinic.com.au
eMail: reception@cloudberryclinic.com.au
Maternal Connections: Randwick, Woollahra and Leichhardt.
web: https://maternalconnections.com.au
Justine Adler: 69a Arthur Street, Randwick.
Tel: 0416 088 742
eMail: justine@maternalconnections.com.au
Nicky Abitz: 8 Ocean Street, Woollahra.
Tel: 9018 9299
eMail: nicky@maternalconnections.com.au
Margie Stuchberry: 97 Marion St, Leichhardt.
Tel: 0419 389 519
eMail: margie@maternalconnections.com.au
Mellanie Rollans: Mellanie Rollans has a special interest in working with women and their families through life transitions
related to pregnancy, childbirth, and parenthood, including adjustment, attachment, postpartum
depression and anxiety, and dealing with bereavement.
Dr Mellanie Rollans:
Tel: 0437 864 232
Web: www.drmellanierollans.com
Diabetes Educator:
Amanda Bartlett and Justine Darling are highly respected diabetes educators with a special interest in antenatal nutrition, and have years of experience working in the management of diabetes in pregnancy. They consult in Macquarie Street and Prince of Wales Private Hospital and via tele-health.
I will refer you to Amanda or Justine if you have gestational diabetes or earlier if you wish to see her. The cost of seeing Amanda or Justine is not included in your planning and management fee.
Dietitian:
Linda Cumines: 42 Adelaide Street, Bondi Junction.
Tel: 9359 4694.
Web: https://www.lindacumines.com.au
Natasha Leader: 54-60 Briggs St, Camperdown NSW.
Tel: 0414 520 277.
Web: https://natashaleader.com.au
You do not need a referral to see a dietitian. The cost of seeing the dietitian is not included in your planning and management fee.
Acupuncture Services:
Houng Lau: Eastern Therapies, 2nd Floor Suite 4, 106 Ebley Street, Bondi Junction
Tel: 0400 331 321
Web: www.bondi-acupuncture.com.au
Naomi Abeshouse: The Red Tent, Suite 2/81 Curlewis Street, Bondi Beach
Tel: 1800 733 836
Rebecca Mar Young: The Red Tent, Level1/17 Randle Street, Surry Hills
Tel: 9211 3811
Web: www.redtent.com.au
Brooke Canning & Nicola Marishel: Acupuncture East, 130 Edgecliff Rd, Woollahra:
Tel: 02 9388 9669.
Web: www.acupunctureeast.com.au
Overview of Healthy Eating in Pregnancy
Eating well for pregnancy
Pregnancy is a time when almost all of you will think more about what you are eating. Many of you will wonder what is best for your baby and make changes to the types of food you eat. There are many aspects of diet that need consideration during pregnancy – and I just touch on a few of the most important here.
It’s quality not quantity
You do need to eat extra when you are pregnant, but the amount of extra energy (kilojoules/calories) each day is quite small i.e. equivalent to a couple of slices of bread and a glass of low fat milk only! What you do need more of are nutrients – more B vitamins, folate, vitamin C, iron, protein among others, so it can take some planning to make sure that almost everything you choose to eat is giving you something worthwhile. Don’t worry – I did say almost everything!
One of the simplest ways of achieving this is by thinking about your diet in terms of food groups. Our food groups exist because the foods within each group provide similar nutrients i.e. milk, cheese and yoghurt are all good providers of protein and calcium. There are guidelines to help you to choose the right number of serves from these groups each day.
The benefit of this approach is also that it lets you keep track of your total intake as well as the balance in your diet. It also can help draw your attention to the frequency of those ‘extra’ foods in your diet – the ones that don’t really fit into any of the groups very well. It’s these ‘extras’ that can cause trouble!
High energy, low nutrition = not great for you or bub.
The following table provides a guide as to the amount of food you need for a healthy diet in pregnancy:
| FOOD GROUP | NUMBER OF SERVES | NUTRIENTS |
| Breads and cereals 1 serve = 1 slice bread or ½ cup cereal or ½ cup cooked rice/pasta |
At least 8.5 serves (depends on activity level and appetite) |
Carbohydrate Fibre Folate Vitamin Bs Magnesium Iron Zinc |
| Fruit 1 serve = 1 piece of fruit or ½ cup tinned fruit or small handful dried fruit or ½ cup fruit juice |
2 serves | Fibre Vitamin C Folate Potassium |
| Vegetables Fresh, frozen, canned, cooked 1 serve = ½ cup cooked vegies or 1 cup salad type vegies |
5 serves | Fibre Folate Potassium Magnesium Vitamins: A + C |
| Dairy 1 serve = 250ml milk or Tub of yoghurt or 1 slice of cheese or 250ml soy milk (calcium fortified) |
2.5 serves | Protein Calcium Magnesium Phosphorus Vitamins D + A, B2, B12 |
| Meat 1 serve = 65-80g cooked meat/chicken or 100g fish 2 eggs or 1 cup legumes or 30g cup nuts |
3.5 serves | Protein Iron Zinc Omega 3 B vitamins Iodine |
Provided by Natasha Leader.
Healthy Weight Gain in Pregnancy
Most women should gain between 10 and 15 kg during the pregnancy. About half of that is from the baby, the amniotic fluid, the placenta and the womb. The other half is extra fat stores, blood and other fluids and breast development. If you gain too much or too little weight it may affect the pregnancy. If you gain more than 15 kg it may be difficult to lose the weight afterwards.
Your ideal weight gain depends on your starting weight or body mass index (BMI), which is your weight in kilograms, divided by your height in metres multiplied by itself (weight/height2):
| Weight status | BMI | Ideal Total Weight Gain |
| Underweight | < 18.9 | 12.5 – 18 kg |
| Normal Weight | 19 – 24.9 | 10 – 15 kg |
| Overweight | 25 – 29.9 | 7 – 11 kg |
| Obese | 30 – 34.9 | 3 – 7 kg |
| Morbidly obese | > 40 | 0 – 4 kg |
Watch your weight gain, by Certified Dietitian, Natasha Leader:
Everyone is different and weight gain will always vary between women, but it is important to keep an eye on it. A higher weight gain can lead to complications that are potentially avoidable. In the women I regularly see who have gained an excess amount of weight, a diet history usually reveals the culprits are high calorie snacks and bigger portions at meals. Portion size is a vital part of weight management.
If you are hungrier and are already eating the recommended amounts of protein/starch already then the best way you can bulk out a meal is by adding vegetables – while the other meal components may be nutritious, if you’re overdoing it you’re more likely to put on too much weight. A quick way to think about it is by using the ‘plate’ model. Half your plate should be salad or cooked vegetables, then a quarter lean protein (meat/chicken/fish/tofu/eggs), and a quarter starch (bread/rice/pasta/quinoa or noodles).
My five top tips
1. Choose high fibre breads and cereals
2. Choose low fat dairy products
3. Choose lean meats
4. Eat more vegetables
5. Choose your snacks wisely
It’s all in the planning
If you are feeling sick often the last thing you feel like doing is thinking or talking about food but spending a short time focusing on your shopping list and planning ahead will help a lot in managing your diet. Ensuring you have nutritious snacks on hand and a list of options for work lunches as well as perhaps some weekend cooking to enable quick but healthy dinners through the week will save you from the trap of banana bread, giant sandwiches and late night laksas!
It isn’t always easy, but it is worthwhile
The potential changes to your appetite, nausea plus cravings and food aversions along with early fatigue make it a trying time for you – not to mention the food safety restrictions and conflicting information you might read.
If need be I am happy to see you during your pregnancy, to work with you to answer any queries you may have. I aim to provide some practical help in managing any of the above considerations, as well as looking at the adequacy and balance of your diet. We can also focus on any planning, shopping, label reading and cooking issues you may have!
https://www.myhand.com.au
Diet and Exercise
I recommend that you take a pregnancy supplement during your pregnancy, that includes Iron and Folic Acid, such as Elevit, Tresos Natal, Kin, MyGen, or Blackmore’s Gold. In Natal make a supplement with and without iron. Consider fish oil supplements, which may reduce the risk of early birth.
Iron deficiency is very common in pregnancy. The symptoms include tiredness and lack of energy. Iron deficiency may affect your recovery from birth and your milk supply. I shall check your iron stores at times during the pregnancy and will recommend a supplement if you are deficient. The highest dose supplement is Ferro Grad C, however it can be quite constipating, in which case Maltofer syrup or tablets, or the liquid Spatone may be better options, although it gives you a much lower dose of iron. Do not take Iron at the same time as tea, coffee, Calcium or dairy, which inhibit iron absorption.
If you are very iron deficient or do not tolerate or respond to oral supplements (or would just prefer it) then I can arrange an iron injection, known as Ferinject or Monofer It is given intravenously, and takes about an hour. It costs $45 with Medicare. Iron infusions are performed in the infusion clinic, or some GP surgeries. There is a small risk of allergic reaction, skin staining or low phosphate levels.
Vitamin D deficiency is common. I recommend you have 15 minutes of sunlight every day, preferably early morning or late afternoon, and you may need a Vitamin D supplement, such as Ostelin. Iodine deficiency is also surprisingly common in Australia and there are usually no symptoms. It is recommended that all women who are currently pregnant or planning a pregnancy take a supplement, containing 150mg iodine, throughout pregnancy and while breastfeeding.
I shall provide you with a booklet that gives you details about foods to choose and foods to avoid in pregnancy. And although you are eating for two during pregnancy, this does not mean twice as much! On average you should expect to gain 10-15 kg in weight during the pregnancy. In pregnancy you have increased insulin resistance, so it is preferable to choose low glycaemic index (GI) foods, and reduce your intake of saturated fats, processed foods and white sugar, white flour and white rice.
You should aim to have three meals per day, each with some lean protein, starchy carbohydrate and green vegetables. You should also have three snacks per day in between meals. All meat and seafood should be cooked through. Soft cheeses, patés, and smoked or cured meats should be avoided, unless they are then cooked, in which case they are fine. All dairy should be pasteurised. Caffeine should be restricted during pregnancy. One coffee per day, however, is reasonable.
The current recommendation on alcohol is to avoid it entirely during pregnancy. That is because heavy or frequent alcohol consumption in pregnancy has been associated with a range of problems with babies including birth defects and a risk of alcohol dependence in later life. The official advice used to be only one alcoholic drink per day, but this has been reduced to none, because we do not have good evidence on what the safe threshold is. If you are going to drink alcohol during pregnancy then my advice is to limit it to a single standard drink, no more than one or two times per week.
Cigarette smoking during pregnancy has been shown to cause a variety of problems for both you and your baby. I recommend you to cut down or, preferably, quit smoking or vaping as soon as you find out that you are pregnant, even if you need to use Nicotine patches to help you through the pregnancy. You should encourage your partner not to smoke, as it is then easier for you not to smoke, and smoking in the home increases the risk of SIDS and childhood respiratory diseases, including asthma.
You should try to remain active during the pregnancy. Most exercises are fine, including brisk walking or even light running and upper body exercises. Swimming and aquarobics, in particular, are great. Core strength and breathing exercises, such as pregnancy yoga and Pilates are also excellent, as are classes that develop your breathing and stretching techniques.
You should avoid sit-ups, crunches and exercises that increase abdominal pressure or separation of the abdominal muscles. And it is important you keep your heart rate under 140-160, depending on your level of fitness, and, above all, not to over-heat. Remember the baby takes up a lot of your heart and lung reserve, so please do not to push yourself too hard in pregnancy. Please make sure that you drink plenty of water before, during and after exercise, especially in summer.
Good Bowel and Bladder Habits
These are important for long-term bladder and bowel function, and include:
• Drink 1.5 to 2.5 litres of fluid each day, preferably water and not flavoured drinks
• Empty your bladder up to eight times per day
• Take your time — don’t hurry or strain to empty bladder or bowel
• Sit properly on the toilet with feet flat on the floor — don’t hover or dangle legs,
• Maintain bladder capacity — no ‘just in case’ visits to the toilet
• Do at least three pelvic floor exercise sessions each day, and ideally four or five: 10 x 10 seconds
• Brace by squeezing your pelvic floor before lifting anything, eg a toddler, baby, washing or pram, or
before coughing & sneezing.
Keeping Fit and Healthy
It is important to maintain your fitness with regular, gentle exercise throughout your pregnancy. Exercise programs that include walking or aqua-aerobics are ideal. Utilise the pelvic floor “bracing” technique to protect your body throughout each exercise session.
You are free to continue with your regular non-contact sports for as long as you are comfortable doing so. However, if you experience any pain or discomfort during any exercise activity, be sure to stop the activity and seek professional advice. Starting new sports or participating in vigorous exercise should be avoided while you are pregnant. Contact sports especially should be avoided, particularly after you are 13 weeks (4 months) pregnant.
Preparing Guidelines for Exercising Safely
Exercise in specially designed classes
• Avoid exercising in the heat or for prolonged periods
• Avoid eating in the hour immediately prior to exercising
• Drink plenty of water before, during and after exercising
• Go to the toilet before beginning exercising
• Begin with warm-up—large, free body movement and stretches, and finish with a slow cool-down,
including stretches
• Always get up slowly when rising from the floor. Lie fully on your side before you get out of bed
• Don’t push through any pain or discomfort — use alternative exercise
• Exercise at your own pace — rest if tired or short of breath
• You should be able to maintain a conversation as you exercise i.e. NOT short of breath
• Never exceed heart rate of 160 beats per minute, or less if you have a slow exercising heart rate
• Wear cool, comfortable, supportive clothes that allow freedom of movement. Bike pants or tights, a
good bra and sports shoes to support the arches of the feet are recommended
Avoid:
• spending any time lying flat on your back
• any “sit-ups” or abdominal “crunches” exercise while pregnant
• rapid, alternating movements any high-impact activities Seek further help if you experience any of the following:
• Pelvic Joint Pain — Pubic Symphysis, Sacro-Iliac Joint (SIJ) or “Sciatica”: Grinding/grating, severe aching, sudden stabbing pain, unable to take weight, limping, muscle spasm, pain on movement including walking, pain on lifting one foot up, such as putting shoes or underwear on.
• Rectus Diastasis — Separation of the abdominal muscles: A bulge appears in the central line of the abdomen as you get up, change position, lift, or cough.
• Back pain: Lumbar (low back) pain, thoracic (mid back) or neck pain
• Bladder control problems — Accidental loss of urine with cough, sneeze or laughing
• Constipation – difficulty or straining to empty the bowels – this is also bad for pelvic floor
• Carpal Tunnel Syndrome — Numbness, pins and needles, tingling or pain in the fingers and hand or wrist, often worst in the mornings, and sometimes settling with a wrist splint or injections
• De Quervain’s tenosynovitis – painful inflammation of the tendon in the wrist, near the thumb. May need surgery. See https://www.myhand.com.au
• Localised muscle tension or cramps. May settle with Magnesium supplements, which are safe.
Pelvic floor muscle exercises
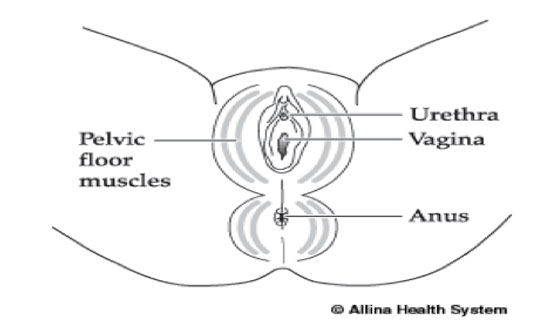
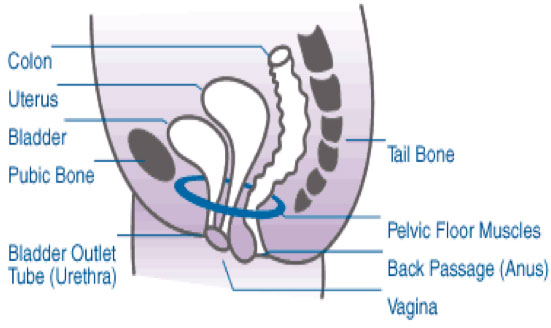
The pelvic floor is made up of a sling of muscles and connective tissue. They stretch like a hammock from the pubic bone at the front to the tailbone at the back. The three openings (urethra, vagina and rectum) pass through the pelvic floor muscles. Strong pelvic floor muscles help prevent leaking of urine, wind and faeces. They also play a part in sexual function and stability of the spine.
One in three women who have had a baby will experience some leakage of urine after the birth. This may be prevented by strengthening the pelvic floor both before and during pregnancy, and after your baby is born. By practising pelvic floor strengthening exercises regularly you can help ensure these muscles stay strong. All women should continue doing pelvic floor strengthening exercises daily in order to prevent pelvic floor weakness in later life.
To activate and strengthen your pelvic floor muscles, position yourself by either sitting up tall or lying on your side. You should feel comfortable in whichever position you choose, with your back in a “neutral” curve and your tummy, buttocks and thighs fully relaxed. Gently draw your pelvic floor muscles up in a “squeeze and lift” action by imagining you are stopping the flow of urine. At the same time continue to breathe easily. This will close off and draw up the muscles around your vagina and back passage.
Aim to hold this contraction for up 5-10 seconds, then relax for 5 seconds. Make sure you are not squeezing your buttocks or bearing down or straining in any way. Repeat this action up to 10 times. You can further progress to performing 10 short, fast, and strong contractions Performing this set of exercises at least four to five times daily will help you to maintain good bladder control, or help improve your control of your bladder if you find urgency or frequency is a problem. It is a good idea to “brace” with these muscles before you lift, move, cough, laugh or sneeze.
If you find you cannot activate these muscles, are holding your breath or seem to be straining, stop performing the exercise and talk to your physiotherapist. Regular pelvic floor exercise is important in pregnancy, but you need to make sure your technique is correct. Additionally, it’s important not to stop the flow of urine mid stream repeatedly as an exercise, as this is not good for your bladder.
Antenatal Visits
As your pregnancy progresses, the frequency of your visits will increase, in order to check on the wellbeing of both you and your baby. This is particularly important at the end of the pregnancy.
A pregnancy lasts 40 weeks on average, so you will have 10–12 visits with me during this time. At your second visit I shall provide you with an antenatal card. This card contains all your important pregnancy information at a glance, so please carry it with you all the time and bring it to all visits.
Please feel free to bring your partner to the visits, especially your first visit. Children are welcome as long as they have no cough, cold or runny nose. Also, if your child distracts you during a visit, you will get less benefit from the consultation. Since the COVID-19 outbreak I have stopped providing toys.
Most of your appointments are schedules for 15 minutes. I always try to run on time, however the very nature of obstetrics means that I can be called away suddenly, and also that I may unexpectedly need to give extra time to a patient with an unanticipated problem. I recommend that you call an hour before your appointment to confirm that I am running on time. If you are more than 5 minutes late I may need to reschedule to avoid impacting other patients.
Your first visit.
This is often the longest, lasting 45-55 minutes, and usually occurs at around 8 weeks. This is what you
can expect during your first visit –
* I shall take a history, check your weight and blood pressure and, if necessary, do a Pap test. A
physical examination, may be recommended, depending on past or family history.
* I will perform a dating ultrasound if required – you will need to have a comfortably full bladder. If the
pregnancy is difficult to see, especially in very early pregnancy or your bladder is not full or if your
uterus is retroverted (tilted backwards), I will need to perform an internal (vaginal) ultrasound.
* I will review your results or order your booking blood tests, if they have not already been done
* I shall give you a pregnancy pack and a booking form for either POWPH or RHW and a “to do” list.
* We will discuss your plans, expectations and any special needs you may have during the pregnancy
and I shall organise any further investigations.
13 to 14-week visit
During this visit I shall check the results of your NIPT and early structural scan or first trimester screen, if you have had one.
17 to 18-week visit
I shall check that your pregnancy is progressing well, as you will probably not have started to feel movements yet, especially if this is your first pregnancy, or the placenta is at the front. I shall also arrange for your 20 week “morphology” ultrasound, if this has not already been booked.
20 to 22-week visit
I shall discuss the results of your 19-20 week ultrasound scan. You should have your long (1 hour) appointment with Bridget around this time if it is your first baby.
24 to 25-week visit
I shall give you a referral for your diabetes screening test, as well as your blood count and iron stores,
and make sure you have had or booked an appointment with my midwife, Bridget.
28 to 29-week visit
I shall discuss the results of your diabetes screen and other tests. You need to book a 3D scan. You should have a whooping cough (Pertussis) booster with your GP or family doctor at 30 weeks.
34 to 36-week visit
I shall repeat your blood tests to check your iron stores, if necessary. Consider the RSV vaccine now.
36-week visit
I shall perform a vaginal-perineal swab test, to screen for Group B Streptococcus. I also recommend a 36 week growth and well-being scan. You may wish to have a second, visit with my midwife.
37-week visit
I shall review the results of your swab test. If it is positive (20% of women) you will need intravenous antibiotics in labour, and sometimes oral antibiotics beforehand. I shall also review the results of your 36 week growth scan. If your baby is much bigger or smaller than usual I may need to arrange further monitoring, including extra scans. I shall discuss your plans for birth in the lead up to this visit.
Advice on Pregnancy Sickness
Many women experience nausea in early pregnancy and some women experience vomiting. Although often referred to as morning sickness the feeling of queasiness can last all day.
The symptoms occur in part because of your levels of pregnancy hormone, which is why they may be stronger with twins, but can also be affected by your background mood, your feelings and other factors. For severe symptoms and weight loss you may need to be admitted to hospital for intravenous fluids.
In general the symptoms get worse until around 8-10 weeks then level off, and then usually improve from around 12-13 weeks. Some women experience nausea symptoms throughout pregnancy and even when the nausea settles there may be days on which the nausea symptoms return. Fortunately nausea is generally associated with good pregnancy outcomes, although some women may have a normally progressing pregnancy with no nausea symptoms. Some women may have nausea of pregnancy even when the pregnancy is not progressing, so a dating scan at 8 weeks is recommended.
How to Manage Nausea Symptoms:
1. Avoid the Triggers: especially big meals, rich food, spicy food, fatty food, or long gaps between food
2. Settle the stomach:
• Start the day with a cracker or dry piece of toast even before getting out of bed
• Snack or graze constantly or frequently throughout the day
• Favour carbohydrates – crackers, toast, pasta, rice
• Ginger, either fresh or in tea, drinks or lollies
• Keep hydrated by sipping water or sucking on ice cubes
3. Over the counter medication:
• Ginger (Zingiber) and Pyridoxine (Vitamin B6).
• Doxylamine (Restavit) – this is an antihistamine and very safe in pregnancy. It is recommended by Mothersafe, so do not be put off by the “Do not use in pregnancy or breastfeeding” label warning. NB Doxylamine is very sedating, especially when you take it for the first time, and can make you feel groggy, even the next day. Try taking ¼ tablet morning ¼ tablet lunchtime and ½ tablet evening.
4. Prescription medication (For these you need a script from me or from your GP):
• Metaclopramide (Maxolon/Pramin): take one tablet half an hour before meals. Helpful for nausea but too late if you are already vomiting. I have intramusculat injection form I can give in my rooms.
• Ondansetron (Zofran): these tablets or wafers, that you can dissolve on your tongue, are very effective, but are very constipating. They are designed for chemotherapy sickness but are safe.
5. Control Reflux:
• Antacids are first line: eg Mylanta, Gaviscon, TUMS, Rennies – all may help.
• Nizatidine (Axid) is second line and available on prescription
• Rabeprazole (Pariet) is third line and available on prescription. Nexium is available over the counter
• Avoid lying down or brushing teeth immediately after eating
6. Acupuncture works well for some women:
• Houng Lau, Eastern Therapies, 2nd Floor, Suite 4, 106 Ebley St, Bondi Junction. Tel 0400 331 321
• Red Tent, 2/66 Hall St, Bondi. Tel: 1800 733 836 and L1,17 Randle St, Surry Hills. Tel: 9211 3811
• Acupressure or travel wrist bands work for some women and may be worth trying
7. Hospitalisation for severe intractable nausea and vomiting:
• The best option if you cannot even keep water down or have lost a lot of weight
• You can be admitted for the day for intravenous fluids and medication, but can incur an expense
• Sometimes you may need to stay overnight or even for a couple of days.
Long Haul Flight Advice
Issues:
1. Water: drink only safe, bottled water. Keep well hydrated.
2. Food: eat freshly cooked and properly cooked food. Avoid street food, buffets and raw or under-cooked food. Be careful of ice in drinks.
3. Radiation: you are exposed to a small increase in the amount of exposure to background radiation
4. Security: consider not only the customs and safety of the country you are visiting, but remember motor vehicle accidents are the leading cause of injury in people undertaking overseas travel
5. Travel Insurance: make sure your travel insurance specifically covers you for any pregnancy related complications
6. Insect-borne infections: reduce your risk of mosquito and other infections by covering up, wearing DEET, using air-conditioning and avoiding dawn and dusk, which are common biting times
7. Respiratory Infections (including COVID-19): airports are hubs of infection. I recommend wearing a mask while in transit through airports. You should assume that the “Flu” and COVID are all around you
8. Travel Letter: make sure you get a letter from me or from your GP dated within 10 days of your departure (required after 28 weeks)
9. Access to Help: you may have limited access to help while away. I will be unable to help you in the same way as if you were in Sydney
10. Deep Vein Thrombosis (DVT): long haul while pregnant travel increases your risk of blood clots in legs or lungs, which can be serious
Strategies to reduce the risk of deep vein thrombosis:
Do:
• Consume plenty of drinking water;
• Use full length, surgical grade, stockings for the entire flight and until you are fully mobile;
• Walk around the cabin or up and down the aisle every 2-3 hours;
• Wiggle your toes frequently when seated.
Don’t:
• Consume anything that de-hydrates you, especially caffeine or alcohol.
Management of Constipation in Pregnancy
Background
• Constipation is a common problem during pregnancy
• Constipation is more common if you start taking iron supplements, especially Ferro Grad C
• Constipation is more common around the time of birth whether you labour or have a caesarean section
• Constipation is more common if you are dehydrated
• Constipation is more common if you are less mobile than usual
• Constipation can cause other problems, including haemorrhoids, anal fissures, and pelvic floor weakness, leading to urinary incontinence and pelvic organ prolapse, usually in later life
Prevention is the key:
• Drink plenty of water every day and reduce/avoid caffeine and sweetened drinks or juices
• Have more fresh fruit and crunchy vegetable every day, such as pears, prunes, broccoli and spinach
• Have less processed food, such as white sugar, processed white rice, processed white flour and choose more complex carbohydrates, such as whole grains
• Try adding a little fibre, if you need to, such as Metamucil
• If you are controlling your sugars you can try Benefibre instead of Metamucil, Soy and Linseed bread instead of white bread and low GI fruit such as strawberries instead of watermelon
Treatment – all available over the counter:
• Start with Movicol – one sachet twice daily
• Add Coloxyl – I usually recommend avoiding Senna, as it can cause bowel cramps – two per day, if
• Movicol not successful after 1-2 days
• Add Lactulose – 20 mls twice daily
• Second Line Treatment:
• Try Glycerine suppositories: insert one suppository into your back passage every 8 hours if Coloxyl not successful after 1-2 days
• Try Microlax enema insert contents into your back passage if Glycerine not successful after 1-2 days
Emergency Treatment:
In an emergency, if you have been unable to open your bowels and you are in significant pain please go to the emergency department at Prince of Wales Hospital, or your nearest emergency department. You may need procedure, known as manual disimpaction.
Information on Diabetes Testing in Pregnancy
Background
Nearly 10% of pregnant women will develop gestational diabetes (GDM). Around 50% of women with GDM will develop Type 2 diabetes in later life (10 years after pregnancy), and late diagnosis can result in lasting damage to your eyes, kidneys and nerves. GDM can have effects on the pregnancy, but often these are often mild, and can usually be minimised by good control of your blood sugar levels, often with diet and exercise alone. Some women need tablets or insulin injections. Babies born to women who have GDM have a higher chance of developing heart disease and diabetes in later life.
Early Testing
If you are at increased risk of GDM I may recommend an early test at 14 weeks. You are at increased risk for GDM if you are over 40, have had GDM previously, have a strong family history of diabetes, have Polycystic Ovarian Syndrome, have a high body mass index (BMI over 30) or you are from an ethnic group at increased risk of GDM (eg Indian subcontinent, SE Asian, Pacific Islander).
Standard Testing
I recommend a full oral Glucose Tolerance Test (GTT) at 26-28 weeks.
The Test
My preferred provider is Douglass Hanly Moir (DHM), who send me results rapidly and electronically.
To arrange the GTT:
You need to book the test – ring a DHM centre on the back of the form.
You do not need a 3 day high carbohydrate diet if you are pregnant.
You do need a 12 hour fast, so have dinner as normal the evening before the test, and then nothing to eat or drink after 8pm, except water.
You should drink water, so that you do not become dehydrated.
On arrival at DHM you will have a fasting blood test, then a large, VERY sweet drink, then a blood test again at 1 hour and again at 2 hours.
You need to remain there for nearly 21/2–3 hours without doing any exercise.
Management of Gestational Diabetes
If your test is positive I shall arrange for you to see a diabetes educator, to start a diet and exercise programme. You will also be taught how to do finger prick blood sugar level (BSL) testing and keep a record of your blood sugar levels. If your blood sugar levels are high I shall refer you to a physician to discuss starting treatment, which may be either Insulin injections or Metformin tablets.
I shall monitor your baby’s growth, and I may recommend delivery earlier than otherwise planned. You can still plan a vaginal birth if you wish. I recommend you consider antenatal breast milk expressing from 36 weeks. After the birth you will need life-long, regular screening for Type 2 diabetes, with your GP.
Information about Twin Pregnancy
How to Manage with a Twin Pregnancy
Twins will require plenty of rest with a twin pregnancy. If you are employed you are likely to need to stop work early and you may need to modify your work environment. It remains important to have a well balanced diet, to keep well hydrated and to do regular, light exercise, including pelvic floor exercises during the pregnancy, although you may find your exercise tolerance is reduced.
Start Aspirin 100-150mg, Calcium 1.2g/day, Folate 0.5-5mg/day, Iodine 150mcg/day and Elemental Iron 80-100mg/day or more. You may benefit from an iron infusion in pregnancy.
You will need a lot of help and support both during the pregnancy, and especially after the babies are born. If you have good family support, it would be helpful to plan to make the most of their help from the outset. This may involve anything from helping with cooking, cleaning, shopping, and minding any other children.
You may need additional support from various community services after the babies are born. These may include services such as Karitane, Tresillian, and Possum Cottage. My midwives will help you after the birth, however I strongly recommend you make contact with your nearest branch of the Australian Multiple Birth Association, which has a lot of resources, practical tips and advice: http://www.amba.org.au
Background
Twins occur in about 1% of pregnancies. The incidence of twins is higher in women taking fertility drugs, such as Clomid or Letrozole, or women undergoing IVF. Pregnancy can be an exciting, but sometimes also an anxious and daunting time, and twin pregnancy doubly so. This sheet is designed to help you to understand what to expect from a twin pregnancy, and to help you prepare for the birth, feeding and being a parent of twins. It should be read in conjunction with the general Information on Pregnancy Care.
Types of Twin Pregnancy
Twins may arise from the same egg or ovum (monozygotic) or from two eggs or ova (dizygotic). Monozygotic twins are identical, whereas dizygotic twins are non-identical or fraternal. Dizygotic twins are far more common, comprising around 80% of twin pregnancies. They usually occur in first or second pregnancies, and are more common in women over the age of 35 and in women with a family history of twins. They may be different sexes and may have different weights at birth, although the weight for each at birth is likely to be lower than for a typical single baby.
Monozygotic twins share the same genetic material, so they are the same sex and have identical features at birth. They are smaller than a typical singleton baby, but their birth weights are usually very similar. Unlike fraternal twins, monozygotic twins are not more common in older women, women undergoing IVF, or women with a family history of twins, and the rate of monozygotic twin pregnancy is fairly constant around the world.
All pregnancies have two layers of membranes around the baby. The inner layer is the amnion and the outer layer is the chorion, which is attached to the placenta. Twins can have separate placentas or a shared placenta. They may have separate chorions (dichorionic) or a shared chorion (monochorionic). Dichorionic twins have two amnions (diamniotic), however monochorionic twins may have separate amnions (diamniotic) or a shared one (monoamniotic).
Most twins are dichorionic diamniotic (DCDA), which is the least complicated form of twin pregnancy. The less common type of twin pregnancy is the monochorionic diamniotic (MCDA) twin pregnancy, while monochorionic monoamniotic (MCMA) twins are rare indeed (1% of twins). Chorionicity is best determined by ultrasound at 10-13 weeks, and should be confirmed by examination of the placenta after the birth.
Symptoms of Twin Pregnancy
Many of the symptoms of early pregnancy are exaggerated in twin pregnancies. These include nausea and vomiting, tiredness or fatigue, heartburn, reflux or indigestion. Your pregnancy hormone (beta-HCG) levels are generally higher with twins.
Many of the symptoms of later pregnancy are also exaggerated in twin pregnancies, including additional weight gain, pelvic pressure and generalized discomfort, backache, muscle and ligament discomfort, excessive fluid around the babies, known as polyhydramnios, swelling of feet, hands and face, stretch marks and skin irritations, varicose veins, and haemorrhoids.
Complications of Twin Pregnancy
Virtually all complications of pregnancy are increased in twins. These include an increased risk of miscarriage, chromosomal abnormalities (including Down syndrome), congenital anomalies (such as limb, heart or spine defects), pre term birth (including extremely pre term birth), blood pressure problems (including pre-eclampsia), diabetes of pregnancy, anaemia, bleeding problems, especially post-partum haemorrhage, discordant (unequal) growth, growth restriction of one or both twins, admission to the neonatal intensive care unit, stillbirth, cerebral palsy, and caesarean delivery for one or both babies.
Moreover, there are some specific complications related to the less common types of twin pregnancy: MCDA twins: twin-to-twin transfusion syndrome (TTTS). This condition varies from mild to lethal and first becomes evident usually between 16 and 28 weeks. Fortnightly ultrasound scans are recommended from 16 weeks until delivery, which is generally 36-37 weeks.
MCMA twins: cord entanglement. This occurs because the babies are both inside the same sac and freely able to move around each other. Cord entanglement can be fatal, but generally occurs late in pregnancy, which is why these twins are usually delivered very early, between 32 and 34 weeks.
Monitoring of Twin Pregnancy
Ultrasound:
An early ultrasound is helpful for dating the pregnancy and determining the twin type. A non-invasive prenatal test (NIPT) and early structural scan are recommended, because of the increased risk of chromosome abnormality. A detailed morphology scan is important at around 19 weeks, to exclude any major anatomical defect. Serial ultrasounds are recommended every 4 weeks for dichorionic twins and every 2 weeks for monochorionic twins, and sometimes a fetal cardiac echo (heart ultrasound) at 18-24 weeks.
Pathology tests:
I recommend the usual pregnancy booking blood tests, as well as an early morning, mid-stream urine sample, to screen for urinary infection and iodine levels. I recommend having a Pap smear if one has not been done within the last two years, and a vaginal swab at 32-34 weeks if you are planning a vaginal birth.
Presenting Position of Twin Pregnancy
| Vertex and vertex: 45% | Vertex and breech: 37% | Breech and breech: 10% |
| Vertex and transverse: 5% | Breech and transverse: 2% | Transverse and transverse: 0.5% |
Timing of Delivery of Twin Pregnancy
| DCDA Twins: 37-38 weeks | MCDA Twins: 36-37 weeks | MCMA Twins: 32-34 weeks |
Mode of Delivery of Twin Pregnancy
Vaginal delivery of twins is safe and reasonable, if that is your preference, provided the twins are dichorionic, appropriately and equally grown, the placenta is not in the way, the leading twin is head down, and there are no major pregnancy complications. Vaginal delivery of twins is one of the few situations in which I do strongly recommend an epidural. The reason for that is the possibility of needing to do an emergency internal manipulation or instrumental delivery of the second twin immediately after the birth of the first twin.
Delivery by caesarean is also very reasonable and possibly slightly safer, if that is your preference, and over 50% of all twins in Australia are now delivered that way. Caesarean delivery is recommended if the twins are monochorionic, the placenta is in the way, if the first twin is not head down, or if there is a major pregnancy complication, such as pre-eclampsia or abruption, or if the second twins is bigger than the first. There are two teams of people at delivery – one for each twin, whether for vaginal or caesarean delivery, so be prepared for a busy delivery room. There will also need to be two sets of neonatal resuscitation trolleys.
Feeding Twins
The midwives and lactation consultants will help you with feeding where required. Breastfeeding twins is a challenge but offers great benefits to the babies. It is common to need some formula supplementation with twins, at least early on. One or both of your twins may need to go to the Special Care Nursery, especially if they are premature, very small, have low blood sugar levels, feeding difficulties or jaundice, or tire easily.
Fetal Wellbeing in Pregnancy
Most of the tests and visits in pregnancy are designed to ensure that your pregnancy is progressing normally and that your baby is well. The most important form of reassurance that your baby is fine is when you are feeling good fetal movements. Most babies have spurts of movement every few hours during the day, which is very reassuring. In late pregnancy babies often squirm instead of kicking.
In the third trimester (after 28 weeks) there should be a 2-hour window every day during which you feel the baby move at least ten times. If you do not then you may need extra monitoring, and possibly even a planned early delivery. I am very concerned about a reduction in the number of movements. If this occurs you should contact the Delivery Suite of your maternity hospital the same day.
I am also concerned about is the development of itch in the third trimester of pregnancy, especially itch without rash and itch on the palms of the hands and/or soles of the feet. If you develop itch during late pregnancy then please contact my rooms immediately and arrange to see me as soon as possible, or after hours contact the delivery suite of the hospital at which you are booked.
Complications in Pregnancy
In early pregnancy the most common problem is morning sickness, which can actually be all day sickness. For most women this gets worse until around 8-10 weeks and then generally gets better after 12-13 weeks. The most important thing is to keep up your fluids, so that you do not become dehydrated. Don’t worry if you lose your appetite for food for a few weeks, you and your baby will both be fine. It is important to remain well hydrated, so if you can’t even keep fluids down and are losing weight then you may need to be admitted to hospital for intravenous re-hydration.
Simple steps to minimise nausea of pregnancy are: avoid large meals, fatty meals, or rich, spicy meals. Start the day with a dry cracker or toast. Have three small meals each day and at least three snacks in between meals. Avoid drinking while eating. Ginger in most forms can help, including the ginger and Vitamin B6 tablets. Acupuncture is of real benefit to some women, but it is not for everyone.
You can try Doxylamine (Restavit): ¼ or ½ a tablet morning and midday, and ½ to 1 in later afternoon. Take with a Pyridoxine (Vitamin B6) tablet with each dose. Both are available without prescription, but Doxylamine is very sedating. If you need stronger medication I can prescribe Maxolon, which is helpful for some women. Otherwise I can prescribe Ondansetron (Zofran), but note it often is very constipating.
The next major challenge in pregnancy is tiredness. In early pregnancy you are often ready to lie down at around 4 or 5pm. You will be especially tired if this is your second pregnancy. Usually you will find that your energy levels improve significantly after about 15 or 16 weeks. That increase in energy should last until around 32-36 weeks, especially if your iron stores are good.
From around 20 weeks of pregnancy you should start feeling fetal movements. From 24 weeks onwards you should avoid sleeping flat on your back. Ideally you should go to sleep on your left side, but sleeping on the right side is better than your back. To help avoiding turning onto your back you may try a pillow or a wedge under your hip. All you need is around 15 degrees of tilt to be safe.
If any complications develop in pregnancy I may need to arrange more frequent visits for closer monitoring of either you or your baby. However, if you need very close monitoring you may be admitted to hospital during your pregnancy. If this is the case, I will look after you during your in-hospital stay. I may need to arrange for extra ultrasound scans and blood tests, and I may need to involve other teams in your care. Most interventions are aimed at reducing the risk of stillbirth. Fortunately, this devastating event is rare, and can be minimised with close monitoring and good care.
With a growing baby inside it is common for you to feel some aches and pains during the pregnancy,
but please ring the Delivery Suite immediately if you experience any of the following:
• vaginal bleeding;
• constant, severe pain;
• a sudden reduction in the number of your baby’s movements after 28-30 weeks;
• itch, especially of hands or feet, and especially after 35 weeks; or
• persistent headache, especially if accompanied by spots in front of eyes, and puffy feet.
For any emergency please ring delivery suite and not my midwife.
My rooms are 20 minutes from the hospital, and I live nearby if I need to attend urgently after hours.
Planning for the birth of your baby
Third Trimester
I shall discuss your birth plan with you. In general, I recommend a “go with the flow” approach, but it is helpful to plan certain things in advance, such as what to pack, and whom to bring for support.
We discuss:
• Syntocinon injection for you, often recommended to help with separation of the placenta, but actually the benefit is to reduce the risk of heavy bleeding (haemorrhage) after the birth.
• Vitamin K injection for your baby, to reduce the risk of internal bleeding (haemorrhage disease).
• Hepatitis B vaccination for your baby, is now usually done immediately after birth.
I recommend all of these injections as routine practice, however, I would be happy to discuss their
benefits in more detail with you during your visits. The Hepatitis B vaccine is the least urgent.
I usually wait for 1-2 minutes before clamping and cutting the cord. I do not recommend waiting longer, as it has not been shown to be of any benefit to term babies, and can result in higher levels of jaundice. If your baby is very jaundiced he/she will require phototherapy, for which he/she may need formula and may need to be admitted to the special care nursery, and therefore be separated from you.
We need to discuss the circumstances under which you may need a ventouse (vacuum) or forceps delivery, an episiotomy (cut to the perineum with scissors) or an emergency caesarean section.
Tests During Pregnancy
Pathology Tests
Booking Bloods and Other Tests
Routine pregnancy booking blood tests include –
• Blood Group and Antibody Screen
• Full Blood Count
• Screening for: Rubella, Syphilis, Hepatitis B, Hepatitis C, and HIV
I also recommend screening for –
• Ferritin (iron) level
• Chickenpox (Varicella), Parvovirus (“Slap Cheek”), Measles and Mumps immunity
• Vitamin D levels
• Thyroid function tests
A mid-stream urine sample, is also advisable, to screen for urinary tract infection.
Triple carrier screening is available for cystic fibrosis, fragile X and spinal muscular atrophy and
now covered by Medicare. Expanded screening (eg Eugene) for over 700 rare inheritable conditions
via cheek swabs from you and your partner at a cost of around $1000. See: https://eugenelabs.com
I shall review your blood tests at your first visit, or organise them, if not already performed by your GP.
A cervical screen (Pap test) is an important five-yearly screening test to prevent cancer of the cervix. I usually perform the cervical screen, as well as a Thin Prep test in pregnancy, if it is overdue.
10-12 Week Blood Tests
The Non-Invasive Pre-natal Test (NIPT), can be performed from around 11 weeks, and will detect Down Syndrome over 99% of the time, as well as other chromosome abnormalities. It can also test the sex of your baby. The turnaround time for testing is around one week, the cost is around $450 and the test needs to be repeated in 1-2% of cases. If the test is abnormal you still need to have an invasive test for confirmation. An early structural scan at 13 weeks is still recommended, to exclude a major structural abnormality.
If you have the first trimester screen, which is the old Down Syndrome screening test, then you will need to have a local blood test as well as the ultrasound scan. The blood test is best done at 10-11 weeks, then the nuchal scan at 12-13 weeks. This option is cheaper but does not detect Down syndrome as reliably. It is a reasonable option if you had IVF with pre-implantation genetic testing.
28 Week Blood Tests
At 26-28 weeks I shall arrange a repeat Full Blood Count, Ferritin and Vitamin D level, as well as a repeat Antibody Screen. If your Blood Group is Rhesus negative, I shall also give you an injection of “Anti D” at 28-30 weeks and again at 34-36 weeks. I shall also arrange a screening test for diabetes in pregnancy. The recommended test is a glucose tolerance test (GTT). If you cannot do the GTT I can arrange a fasting blood sugar level (BSL) after an overnight fast. If your fasting BSL is low you are clear. If your fasting BSL is high you have gestational diabetes and I will refer you to Amanda Bartlett, the diabetes educator, for finger prick testing. If your level is borderline we will have a discussion about the options for further testing, including finger prick testing or the full GTT. Douglass Pathology is preferred.
36 Week Blood Test and Swab
If you are planning a vaginal birth I shall perform a vaginal and peri-anal swab, at 36 weeks, to test for the presence of Group B Streptococcus (GBS). Around 20% of women are GBS carriers, usually with no symptoms. GBS is harmless to adults, however babies can acquire it passing through the birth canal, and can develop a very serious infection. This can be prevented by taking antibiotics in labour, usually Penicillin, so please let me know if you have an allergy to Penicillin, or any other medication. I may repeat your full blood count and iron stores at 34-36 weeks if there has been an abnormal result previously, especially if your iron stores have been borderline or low.
Ultrasound Scans
Your pregnancy is dated from the first day of your last menstrual period (LMP), which is around two weeks before actual conception. I shall confirm this with a dating scan at around 8 weeks. Early (8-10 week) ultrasound scans are generally more accurate for dating your pregnancy than later scans.
At 12-13 weeks you may wish to have a screening test for Down Syndrome (Trisomy 21), known as the Nuchal Translucency Test, if you have not had the Harmony or Generation test. This involves an ultrasound of the baby’s neck and nasal bone. The test is best performed in specialised obstetric ultrasound centres and should be performed in conjunction with a special blood test, done at 10-12 weeks. If these tests show a high likelihood of a chromosome problem I shall discuss invasive testing with you, either Chorionic Villus Sampling (CVS) or Amniocentesis.
I shall arrange for you to have a specialised ultrasound scan at around 20 weeks, known as the morphology scan or fetal anomaly scan. At this scan a detailed review of your baby’s anatomy is performed, to make sure that there is no major abnormality. The majority of major malformations can be detected in this way, as well as some other problems, but please be aware that the background rate of abnormalities is around 3%, and that no single test can detect 100% of problems. It is also important to remember that while we are good at checking fetal anatomy, it is not possible to assess fetal function prior to birth. There is no test for autism, which is not related to Rubella vaccination.
I usually scan your baby at each of your visits, however I usually recommend an external scan at 36 weeks to recheck the baby’s anatomy and to check on the baby’s growth and placental function. I may also discuss further growth scans in the last trimester of pregnancy if I am concerned about the growth or wellbeing of your baby, or if you have high blood pressure or diabetes. If the placenta is low-lying at your 20 week scan, then this will be rechecked with a transvaginal (internal) ultrasound at 36 weeks.
3D scans can provide great views of the baby’s face. The best time to perform a 3D scan is at 30-33 weeks. This is a fun scan and is not medically necessary. If you are unable to attend the 3D scan at 30-33 weeks I will arrange for your 3D scan to be included in the 36 week scan, if possible
Medications in Pregnancy and Lactation
While many medications can safely be taken during pregnancy and breastfeeding, it always helps to ensure that you are on the safest medication and at the correct dose. Mothersafe provides an excellent, free counselling service for women of NSW. Mothersafe also provides fact sheets on safe medications and self-help for common pregnancy complaints, such as nausea, haemorrhoids, constipation, and management of cold and flu. Most cold and flu preparations are safe in pregnancy.
Mothersafe, Royal Hospital for Women:
web: www.mothersafe.org.au
Tel: 9382 6539
Birth Education
If this is your first pregnancy I strongly recommend that you and your partner attend childbirth education. There are many options available, but most are very popular so please book well in advance. Classes include sessions on health education, birth preparation and parenting, and most include a tour of delivery suite. Many classes attract a health fund rebate, depending on your fund.
Prince of Wales Private Hospital runs two classes for women planning vaginal birth: a class on birthing and a class on feeding and settling. They are both helpful. There is a single class for women planning an elective caesarean section, that covers both the caesarean section and feeding and settling.
The following online resources may be of help:
www.birthbeat.com
www.nourishbaby.com
www.childbirtheducation.com.au
https://raisingchildren.net.au
https://firstdroplets.com
Birth Preparation Classes
Carolyn Love: Prince of Wales Private Hospital:
eMail: POWPrivate.Prenatal@healthscope.com.au
Health Education Centre, RHW:
Web: http://www.seslhd.health.nsw.gov.au/RHW/Health_Education/
Calmbirth, RHW:
Web: https://www.trybooking.com/195086
Lynne Hall: Better Beginnings Birth Education Classes and Lactation Consultant
Web: www.betterbeginnings.com.au
Tel: 9664 4315 or 0419 245 966
Jessica Krigstein: private or small group classes
Tel: 0401 959 614
Jane Simons: Physiotherapy Exercise Classes
Tel: 9327 4294
Calmbirth: Karen Mclay, Bowral
Web: www.calmbirth.com.au
Tel: (02) 4871 1806
Shebirths: Nadine Richardson – shebirths.com.au
Tel: 8060 2212
Transition into parenthood/calmbirth:
web: www.Julieclarke.com.au or www.bluemountainscalmbirth.com.au
Parenting for Life: RHW:
Web: https://www.trybooking.com/195174
For Dads:
Beer and Bubs: 1 night session,
Web: www.beerandbubs.com.au
Tel: 9440 9999
The Baby Shed: a hands on workshop for new Dads.
eMail: familysupport@senc.org.au
Web: www.facebook.com/thebabyshed
Dadvice:
Web: www.Dadvice.org
Information on Caesarean Section
Background
A caesarean section is an operation to deliver a baby through the wall of the abdomen, as an alternative to delivering through the birth canal (vaginal or “natural” birth). Caesarean section is now the most commonly performed major surgical procedure in the world.
Indications
Caesareans are usually classified as elective or emergency. Elective caesareans are generally planned. They are performed for reasons such as placenta praevia (where the placenta is in front of the birth canal), breech presentation, twin pregnancy, and for large babies, such as in diabetes.
Caesareans may be performed as an emergency, especially where the labour is not progressing normally, or there are signs that the baby is not tolerating the labour (“fetal distress”), or in the presence of vaginal bleeding. Sometimes the caesarean may be required as a semi-emergency, such as when your blood pressure is uncontrollably high (severe pre-eclampsia).
Timing of Caesarean
The best time for caesarean section is usually 39-40 weeks. The NSW Health Department has stipulated that elective caesarean section should routinely be performed after 39 weeks. This is in contrast to previous practice, when caesarean section was performed at 37 or 38 weeks. Doing the caesarean section near to the due date has significant benefits for the baby, including a 50% reduction in admissions to the special care nursery with breathing difficulties, or fluid on the lungs.
The latest evidence also shows significant improvement in brain development in babies born later. If your baby needs a caesarean prior to 37 weeks then it is recommended that you have two steroid injections to help the baby’s lung development. This halves the rate of unnecessary nursery admission, although the results of any long-term effects on the baby are not yet known.
Consent for Caesarean
You need to give consent for caesarean, whether it is elective or an emergency. That consent should be freely given, once you understand the risks and benefits of caesarean and the alternatives, and have been given the opportunity to discuss any concerns. The consent form must be signed by you, and nobody else can sign on your behalf. It must also be signed by the person performing the operation, after discussing the risks, benefits and alternatives with you.
Pre-operative Assessment
Prior to caesarean you will need to have blood taken for cross match, in case you need a blood transfusion. We normally check your blood count, and sometimes iron stores, at the same time. The anaesthetist will see you before the caesarean. Some anaesthetists meet you beforehand, but most meet you on the day of the caesarean. At POWPH a nurse or midwife will perform your hospital pre-admission. At RHW this is usually done at the time of admission. Since COVID most pre-admission assessments are done by phone. You may need a COVID test before admission.
Anaesthetic
You will require an anaesthetic for a caesarean section. You can be put to sleep (general anaesthetic) or have a needle in the back that makes you numb from the waist down (regional anaesthetic). General anaesthetic is not usually preferred in pregnancy for safety reasons, so most caesareans are performed under regional anaesthesia, which means you are awake.
There are various types of regional anaesthetic – spinal, epidural or combined spinal and epidural. All involve a needle into the back. A spinal anaesthetic is a single injection that immediately gives a heavy numbness and lasts for around 4 hours. An epidural injection is into the tissue around the spinal cord. It takes longer to start working, but lasts longer, and can be topped up via a tube taped onto your back. It can be used for labour and topped up for caesarean if required.
Each anaesthetist has a preferred type of anaesthetic and it is important to allow the anaesthetist to perform the type of anaesthetic they prefer.
Surgical Preparation
Please ensure that all jewellery is removed prior to going to the operating theatre. Being a surgical procedure, it is performed in a cooled operating theatre, under sterile conditions. The surgeon, assistant surgeon and scrub nurse must all perform a sterile scrub and wear sterile gowns and gloves to prevent infection. Prior to commencing the operation you will have the upper portion of your pubic hair clipped, and a urinary catheter tube will be inserted to empty your bladder. Studies have shown that clipping of hair is associated with fewer infections than shaving with a razor, however having a bikini wax in the days prior to surgery is also a good option. You will then have antiseptic solution, such as Betadine or alcohol, painted onto your abdomen to help prevent infection. Sterile drapes will then be put up to create a sterile field. Please do not touch the sterile drapes at any time. Please let me know if you are allergic to Betadine, alcohol or to tape.
The Procedure
An incision about 12 cm long is made with a scalpel on your ‘bikini line’. I then cut down through the major tissue layers until I reach the womb. The bladder lies over the lower part of the womb, and needs to be pushed down out of the way to reach the thin part of the womb – the lower segment – where I make an incision in the womb big enough to deliver the baby.
I then break the waters, and you may hear the gurgling of the fluid being collected in the suction tube. I then need to deliver the baby through the incision. It is often a tight fit, and I may need to use forceps to guide the baby’s head out gently, which reduces the pressure needed from above. I often hold the baby upside down to help your baby clear the fluid and mucus in the airways.
The umbilical cord is then clamped and cut. I generally like to delay clamping of the cord by one minute, even at caesarean. Because we are working in a sterile field the initial cut must be made by
me, or my assistant, but we generally allow enough cord for your partner to do the final cut. There is a midwife in theatre to make sure that the baby is fine, and to make sure you have a cuddle in theatre. Sometimes your baby has a little fluid on the lung, or needs some minor resuscitation. If you have a caesarean in labour or your baby is pre-term or breech, or if there is any concern about the baby I will arrange for a paediatrician to be present at the caesarean.
Maternally Assisted Caesarean Section (MACS)
If you are having an elective caesarean section and you are very keen to participate in the actual procedure there is the option for you to assist if you are booked at Prince of Wales Private Hospital.
People Present for Caesarean
There are often several people present for caesarean, in addition to you and your partner or support person. I require a surgical assistant, sometime another obstetrician. The anaesthetist requires an anaesthetic assistant. There is a scrub nurse and scout nurse as well as a midwife and often a paediatrician. For preterm babies or twins extra staff members will need to be present.
Recovery from Caesarean
At the completion of the operation you will usually go to the recovery ward for around 30 minutes for observation and monitoring. During that time your baby will usually be brought to you by the midwife, for “skin to skin” contact and for initiation of breastfeeding, if it is an elective caesarean.
Occasionally you will not be able to feed in recovery, in which case at the end of the operation your partner or support person will leave the operating theatre with the baby and midwife and return to the ward. That is a great time for your partner to do “skin to skin” with the baby. Expressed breast milk can be given if necessary. Occasionally elective caesarean may delay your milk supply, in which case frequent feeding or expressing in the first few days may help your milk come to in. For the first 24 hours following caesarean you will generally rest in bed. If you are at POWPH you
can leave your baby in the nursery for a few hours during the night, and I recommend you to make use of this excellent service, firstly to get some rest and secondly because it is difficult to twist and lift the baby. Moreover, I advise you to keep visitors to a minimum while in hospital. It is generally good idea for your partner or mother to stay with you to help, especially on the third night.
Your bladder catheter will usually be removed on the morning following the procedure. If you have had an epidural anaesthetic the epidural catheter will be generally removed at the end of the procedure, having given you some epidural morphine. Your intravenous cannula (“drip”) will be removed when you are drinking adequately, usually the day after the caesarean.
After the first 24 hours it is good to get up and start to walk around. This helps your lungs to re- expand, helps your bowels to re-start, and reduces the risk of blood clots (deep vein thrombosis or DVT). You may need extra pain medication before walking around. By the time you leave hospital you should be fully mobile and should be able to manage stairs slowly.
Bowels can often be slow to return to normal after a caesarean, so I recommend you drink plenty of water, eat a high fibre diet, such as pears and prunes, include some bran or Metamucil, and start Coloxyl tablets early, to help your bowels to start moving. Movicol sachets can be added. You will generally be in hospital for four or five nights following caesarean section. If you are planning to breast feed then this time is valuable to become confident with feeding and settling, which is often a major challenge for first time mothers.
Your recovery time is around 6 weeks. I advise you not to drive for the first three to four weeks, or until you can safely perform an emergency brake procedure. You should not perform any heavy (more than 10kg) lifting for around 3 months. You should avoid sit-ups or crunches for 3-6 months following either natural or caesarean birth, to allow the abdominal muscles to knit.
Complications of Caesarean
Caesarean section is a very commonly performed operation and it is extremely safe for both you and your baby. It is, however, a major operation, and no operation is entirely without risk. The most common risk is infection, either in the skin, under the wound, in the lining of the womb (endometritis) or a bladder infection. It is normal for some bleeding to occur at all births, but is typically heavier at caesarean than at natural birth. Sometimes the bleeding can be so heavy during caesarean section, that you require blood transfusion and special procedures to stop the bleeding.
Other risks include the risk of blood clots (DVT) in legs and lungs, for which you will be given surgical stockings and daily injections of a type of Heparin, known as Clexane, to thin your blood until you leave hospital. Following the procedure scar tissue will form in the skin and in the tissue below. The skin scar can become thick and heaped up, known as keloid. The deep tissue scarring can make future operations more difficult. In general each caesarean becomes a little more difficult, in contrast with natural birth, which generally becomes easier after the first birth.
Uncommon complications include the possibility of injury to bladder or bowel or the ureters – the tubes from the kidneys to the bladder. In rare cases, such as where the placenta is abnormally stuck to the wall of the womb, the haemorrhage can result in the need for an emergency hysterectomy (removal of the womb). This is only performed as a life-saving procedure.
You should call the Delivery Suite if you experience fevers above 38 degrees, any obvious infection, worsening pain or bleeding, chest pain, breathlessness, calf pain and swelling, or difficulty emptying your bladder within 6 weeks of the operation. You will need to come in for assessment. That may be either to Delivery Suite or to the Emergency Department.
Following caesarean you should generally wait at least nine months before conceiving again, and preferably twelve months. If you have had a caesarean it is usually fine to plan for a vaginal birth after caesarean (VBAC) next time if you want one, depending on circumstances. There are, however, issues to be discussed, including a very small risk (under 0.5%) of your caesarean scar tearing in labour, which, in extreme cases, can be life-threatening for both you and your baby.
Pain Relief After Caesarean
If you have a spinal anaesthetic for your caesarean it involves a single needle into your back and there is nothing taped to your back. If you have an epidural or combined spinal and epidural there will be a plastic epidural catheter taped to your back for the duration of the procedure. At the end of the caesarean the epidural catheter tube will be removed from your back.
Thereafter we rely on tablets for pain relief. Usually we use a combination of:
• Panadol or Paracetamol: while paracetamol alone may not be effective in controlling pain, it is much more effective when taken regularly than when taken occasionally, and it has been shown to reduce the amount of strong pain killers you need;
• A non-steroidal anti-inflammatory pain-killer, such as Meloxicam (Mobic), Diclofenac (Voltaren) or Ibuprofen (Nurofen): these are very effective in conjunction with paracetamol. These medications can cause irritation of the stomach and even ulcers, so they should not be used for more than 7-10 days and they should always be taken with food. You must avoid them if you have Crohns Disease or Ulcerative Colitis, or other conditions involving ulcers;
• Long-acting Opioid, such as Targin, or Tramadol Slow Release: these morphine-based pain killers can be very effective for pain relief for the first 2-3 days following caesarean section. They are very strong and should usually not be continued beyond day three.
• Short-acting Opioid, such as Oxycodone (Endone) or Tramadol: these morphine-based pain killers can be very effective for the relief of breakthrough pain when the baseline pain killers wear off or do not adequately control your pain. They generally come in two strengths and we would usually try the lower dose first, knowing we can increase the dose if necessary.
At discharge I recommend:
• Regular Paracetamol for 7-10 days
• A non-steroidal anti-inflammatory tablet with food for up to 3 days, if necessary;
• A short-acting opioid, such as Endone, if needed, occasionally for breakthrough pain.
Fees for Caesarean
In private medicine the fees are set by the provider, but you should have informed financial consent, which means you should know in advance approximately what they will be. My fees are unchanged, even if you need a caesarean in the middle of the night.
The fees for caesarean are generally similar to the usual obstetric fees, except you will need to pay for a surgical assistant. The surgical assistant fee can vary greatly. The usual surgical assistant fee is around $700-$800 and you generally get back a total of $120 from Medicare and your fund.
Many professional fees vary greatly, and also change from time to time, so it is difficult to give you a precise figure but a guide to your out of pocket expenses is as follows:
• anaesthetist from $800 to $1,600;
• surgical assistant around $700 usually, but can be as much as $1000;
• paediatrician around $600-$800.
Please note that if you require an emergency caesarean after hours or at weekends then these professional fees may be increased, although my fees remain the same.
If you have an epidural for labour and then an emergency caesarean you will receive two anaesthetic bills.
Hospital fees, including tests and medications, may be covered by your fund, depending on the cover you have.
Please check these costs with your fund prior to booking into the hospital. Please also check that your baby will be covered in the event of an admission to the neonatal nursery.
Preparation for Caesarean Birth
In the second half of the third trimester I start to have discussions with you and your partner, regarding your birth plan. My aim is to help you achieve the birth experience you would like.
If you are planning a caesarean birth I generally like to book it in well ahead of time. My operating list is every second Friday at Prince of Wales Private Hospital. I have access to operating lists on alternate Wednesdays and some Fridays at the Royal Hospital for Women.
Timing of Birth:
The safest time to give birth is usually between 39 and 41 weeks, however the ideal time varies according to factors such as maternal age, blood pressure, fetal growth, diabetes, and IVF. Prior to 39 weeks, babies may have more fluid on the lungs and therefore may have more breathing difficulties. Generally I would try to get to at least 39 weeks if we can. Most elective caesarean sections are scheduled for 39-40 weeks.
At the other end of the spectrum I would recommend not waiting too long after your due date, although ultimately we have to make a decision that feels right for you. The stillbirth risk starts to rise very slowly from 38 weeks, and somewhat more steeply from 41-42 weeks, and earlier if there are risk factors. Babies are fully developed by 40 weeks and there is little to be gained from waiting longer from the point of view of your baby’s development. The longer you wait the greater the chance of going into labour.
Elective Caesarean Section:
Prior to the caesarean section I will arrange an anaesthetist, a surgical assistant and a paediatrician. Please let me know if you have a preference for paediatrician.
You will need to sign a consent form prior to caesarean section, and where possible I will discuss the details and ask you to sign the consent form in advance. It would be helpful if you have read my booklet on caesarean section.
The hospital will perform pre-admission check by telephone prior to the caesarean section, and confirm what time you should come in to hospital. You should not have any food for six hours prior to the caesarean section time. You can have water only until two hours prior to the caesarean. You should come in to hospital 90 minutes prior to the caesarean start time. At POWPH you can sip till they send.
Emergency Caesarean Section:
A caesarean section that is performed in labour is known as an emergency caesarean section. If you go into labour prior to your planned caesarean section I will need to discuss with you whether to try for vaginal birth or to perform and emergency caesarean section. For that we will need to transfer you to the operating theatre and a theatre team will need to be called in, including an anaesthetist, a surgical assistant and a paediatrician or midwife experienced in newborn resuscitation, and you will need a cannula in your hand or arm and blood taken for cross match, in case you need a blood transfusion.
You will need to sign a consent form prior to caesarean section, and where possible I will discuss the details and ask you to sign the consent form in advance. It would be helpful if you have read my booklet on caesarean section, in case one is required in an emergency.
Post Partum:
Two issues I would like you to consider are for just after the baby is born. The first is the Syntocinon injection that we give you very soon after the birth. It is often said that it is given to speed up the delivery of the placenta but that misses the real point of the injection, which is to reduce your risk of excessive bleeding after the birth. Having the injection halves your risk of post partum haemorrhage. Your blood is precious. Having spent much of your pregnancy trying to maintain good blood and iron stores it makes good sense to have the injection. The second is the Vitamin K injection. This injection helps prevent a rare but potentially serious bleeding disorder, that can cause bleeding in your baby’s brain. The Hepatitis B vaccine for the baby is generally given at the same time as the Vitamin K injection.
Generally you are in hospital for four or five nights after the caesarean. If this is your second or subsequent baby and you successfully breast or bottle fed last time you may wish to leave hospital a little earlier this time. This may apply especially if you are not allowed to bring any other children or family members into hospital.
Feeding and Settling:
For many first time mothers feeding and settling can be a challenge. Most babies do not naturally attach to the breast, they often attach to the nipple. If that is not corrected quickly then it will cause nipple damage, which can be very painful, and take a while to heal. It is important, therefore, for both you and the baby to learn good technique from the outset. Hydro-gel pads (or Lansinoh cream) may be of help.
Please take advantage of the expertise and support offered by the midwives on the ward. If necessary, you can be referred to a Lactation Consultant. There are daily drop-in classes, lactation consultant sessions and one-on-one sessions during the week, and sometimes even at weekends, depending which hospital you are booked at.
Your milk generally comes in on day three or day four, but can take up to one week, and occasionally even longer. When it comes in you may be quite tearful. Most babies lose between 5 and 10% of their birth weight in the first few days. If your baby loses much more than 10%, then you may need to supplement the breast milk with some formula, especially if your baby is jaundiced, or low birth weight to start with. This is something that you will be given advice on by your Paediatrician, in conjunction with the Midwife or Lactation Consultant.
When you go home remember to send a text to my midwife, Michele (or Chantelle), who will arrange to do a telehealth home visit, to make sure that the feeding and settling is going well. important service, and one that I am very proud of, so please take advantage of it. This is a very If Michele identifies a need for on-going support she will advise how to go about that, and, if necessary, help to put it in place.
Sleep:
By far the most difficult challenge facing new mums is coping with sleep deprivation. Before the birth please take some time to consider how you personally will cope with sleep deprivation. Most new mums are not prepared for just how difficult it can be to adjust to having a newborn, who, while delightful and engaging in every other way, wants to stay awake all night, and feed, cry, or play, or all of the above.
Most babies will sleep in patches during the day, so please take advantage of every opportunity during daylight hours when your baby sleeps to have a rest yourself as well. If partners or family are around, then they can often take the baby for walks during the day, while you rest, so put them to work.
I recommend limiting visitors to close family, when COVID rules permit. Visitors are well meaning, but often draining at a time when you need all your energy and resources, and above all, sleep. Take advantage of every offer of help from practical things such as shopping, cooking and cleaning, and offload peripheral responsibilities. During COVID-19 restrictions the night nursery at POWPH is closed.
The good news is that there is light at the end of the tunnel. For a while you may feel like there is a heavy fog hanging over you, preventing you from functioning normally and making rational decisions. Over time you usually become more accustomed to broken sleep, and you will learn to take advantage of whatever sleep opportunities you have.
Above all else I think it is important not to torture yourself trying to do things perfectly. Most first time mums especially want to do everything perfectly, and if it works then that is fantastic, but please have a plan B. Sometimes you will need to give your baby formula top ups and that is not dangerous, even if it is not your first preference. Sometimes formula top ups are necessary for a variety of reasons, and your baby will still be healthy and still love you just the same.
Please remember to collect your copy of Dr Howard Chilton’s book, “Baby on Board” and signed bookmark. I may give you a script for pain medications, if you are likely to need them after discharge from hospital, especially at RHW. The POWPH pharmacy dispenses any discharge meds you need.
I look forward to finishing this journey, and remember, it will all be worthwhile when you are holding the little one in your arms.
Maternally Assisted Caesarean Section:
If you are booked at POWPH and having a planned caesarean and you are highly motivated to assist with the birth please let me know as this will need to be planned and co-ordinated well in advance.
Preparation for Vaginal Birth
In the third trimester I start to discuss your birth plan with you and your partner, following on from our plan at your first visit. You do not need to have a written document, but it is good to be informed, and to have an idea of how you would like the birth to go. It is, however, essential to be flexible, as babies do not always behave as you expect or want them to, both during the birth and afterwards.
My aim is to help you achieve the birth experience you want. If you are planning a natural birth then being in the best physical and mental shape you can be for labour is important. Courses like Calm Birth can be very helpful in reducing anxiety, reducing physical tension, and giving you the confidence to trust in yourself and your body, but they are very focused on drug-free birth and are not suited to everyone.
In general, my aim is to minimise unwanted intervention, but sometimes intervention helps. It is important to remember that the ultimate goal is a healthy mother and a healthy baby. If it takes an epidural or forceps or caesarean section to achieve that, then you should not feel disappointed that your original birth plan did not come about. As much as I want you to stay confident and positive it is important to consider some of the variations to the plan that can happen in labour.
One thing to consider is the need for pain relief. Not all women want or need pain relief for labour, but there are plenty of options from which to choose if you want or need pain relief, including massage, pressure points, warm baths or showers, TENS machine, morphine, nitrous oxide gas and epidural.
Many women choose to have an epidural for labour. Your likelihood of asking for an epidural is reduced if you are highly motivated, or if you have a single support person with you throughout labour, and if you have attended a Calm Birth course or similar. You are more likely to ask for an epidural if your labour is induced or your baby is in an awkward position in labour, or if you have a very long pre-labour.
If you are keen to avoid an epidural, and you are coping well with labour then there is absolutely no reason to have one. You get a natural high from the adrenalin and endorphins during the labour and after birth, and you can quite rightly feel a strong sense of accomplishment after successful vaginal birth, particularly if you have achieved it without an epidural.
On the other hand, there is no shame in having an epidural, if you want one or need one. Some women know in advance that they want one. Other women know that they do not want one. Many women want to wait and see. An epidural may well help if your labour is progressing slowly, and this commonly occurs if the baby is in a posterior position, i.e. head down but looking upwards, so-called “star gazing”. If the baby gets distressed or baby gets stuck and your cervix is not fully dilated (10cm) then I shall do an emergency caesarean section. If the baby gets distressed or baby gets stuck and your cervix is fully dilated and if the head is low in your pelvis then I will do a ventouse (vacuum) or forceps delivery, if the head is low enough. You will need an epidural or spinal for a caesarean, and I generally recommend an
epidural or pudendal block for a forceps delivery, and sometimes for a ventouse delivery.
Timing of Birth:
The safest time to give birth is generally between 39 and 41 weeks, however the ideal time varies according to factors such as maternal age, blood pressure, fetal growth, diabetes, and IVF. Prior to 39 weeks, babies may have more fluid on the lungs and therefore may have more breathing difficulties. Generally I would try to get you to at least 39 weeks if we can.
At the other end of the spectrum I would recommend not waiting too long after your due date, although ultimately we have to make a decision that feels right for you. The stillbirth risk starts to rise very slowly from 38 weeks, and somewhat more steeply from 41-42 weeks, and earlier if there are risk factors. Babies are fully developed by 40 weeks and there is little to be gained from waiting longer from the point of view of your baby’s development. Waiting, however, does allow you a great opportunity to go into labour on your own, so again we will make the decision regarding timing that feels right for you.
If you are keen to promote spontaneous labour then cervical sweeps may help you. If all goes well you push the baby out. I will be there at the end of your labour to make sure everything is OK, that your baby is safe, and to help where necessary. Then the fun begins.
Cervical Sweeps:
A cervical sweep is a vaginal examination involving an attempt to insert a finger into the cervix, to try to separate the membranes from inside the cervix in a sweeping motion. A cervical sweep is also sometimes known as a “strip and stretch”. It is a good way of trying to avoid the need for induction. Studies have shown sweeps to be effective in helping labour to come on a week earlier, but you often need two or more sweeps. I usually perform cervical sweeps in my rooms from about 39 weeks.
The sweep can be uncomfortable or sometimes can be painful. If it is too painful I will stop and then we should probably not do sweeps after that. You can usually expect some blood-stained vaginal mucous after the sweep. If I can do a sweep successfully, I often try to do them up to twice each week. Sometimes the cervix is so tightly closed that a sweep is not possible. We can try again in one week.
Induction of Labour:
Induction of labour is a way of making your labour start. Usually labour is induced by breaking your waters, which we do by passing a hook through the cervix and scratching at the membranes until they break. At this point you will feel a trickle or gush of fluid, which will then keep leaking until your baby is born. We then need to start the Syntocinon drip, to help make the contractions start. If you have laboured before, or are already contracting strongly, we may not need to use the drip.
Often the cervix starts off long, closed, hard, and at the back of the vagina. As labour establishes the cervix softens and thins (known as effacement) and, at some stage, starts to dilate. If we are inducing you we need the cervix to be open enough to pass the hook through. To achieve that we bring you into hospital the day before the planned induction to soften and open the cervix, known as cervical ripening. That is done in the morning at RHW and in the evening at POWPH. One or more doses of a hormone, known as Prostin, is given in the form of a vaginal gel, administered by the midwife looking after you.
Pre-labour and Labour:
From the cervix being closed to being 4cm dilated is early labour or pre-labour. This can go quickly or sometimes very slowly. If you are pre-labouring for more than 12 hours, I will offer you the option of having labour induced. Once you are in active labour, which is from 4cm to full dilatation (10cm) labour usually progresses at about one cm per hour. If labour is going slowly you may need a Syntocinon infusion, which is known as augmentation of labour. Once you are fully dilated we sometimes wait for one hour before starting the pushing and most women are pushing for an hour (or more) before first baby is born. Your midwife will generally call me to come in when you are close to having the baby.
Emergency Caesarean Section:
A caesarean section that is performed in labour is known as an emergency caesarean section. If your baby becomes stuck or distressed in labour before the cervix is fully dilated then I will need to perform an emergency caesarean section. For that we will need to transfer you to the operating theatre and a theatre team will need to be called in, including an anaesthetist, a surgical assistant and a paediatrician or midwife experienced in newborn resuscitation, and you will need a cannula in your hand or arm and blood taken for cross match, in case you need a blood transfusion.
You will need to sign a consent form prior to caesarean section, and where possible I will discuss the details and ask you to sign the consent form in advance. It would be helpful if you have read my booklet on caesarean section, in case one is required in an emergency.
Episiotomy:
An episiotomy is a cut with the scissors, usually from the lowest part, or “V” of the vagina, angled to your right side. Episiotomy was once routine. I do not perform episiotomy routinely, but sometimes they are necessary. I try to use warm compresses to the perineum and massage, to reduce tearing during birth. In general, a small tear is better than a cut, but a cut is better than a big or serious tear.
I perform episiotomy whenever I need to use forceps, often when I need to use vacuum, and sometimes for other vaginal birth, especially when the perineum starts to tear early, or becomes very swollen, in which case the skin loses its natural stretch. If you do not have an epidural I will inject local anaesthetic into the perineum before doing an episiotomy, where possible.
Forceps:
You require good pain relief for forceps delivery. Generally this means an epidural anaesthetic. Sometimes I can perform what is known as a pudendal block, which is local anaesthetic injected inside the vagina. This is usually very quick and effective.
I routinely perform an episiotomy with forceps. extending down into the sphincter muscle. This is to reduce the chance of a tear in the midline The importance of such a tear, known as a third or fourth degree tear, is that if it occurs it can leave you with a greater chance of losing control over passing wind, fluid, and sometimes even solids from your bowel. Needless to say, this is personally distressing and socially awkward, but fortunately it is uncommon (3%). Even when it does occur it often improves and sometimes resolves completely with time and good physiotherapy.
Bladder control is often worse after birth. Many women report loss of bladder sensation, and some loss of bladder control after birth, even after caesarean birth. The chance of reduced bladder control is greater if you have had long labour, big baby, ventouse delivery, and especially, forceps delivery.
Ventouse:
A ventouse or vacuum delivery is required if we need to speed up delivery, either because you have been pushing for too long, or if your baby is becoming distressed, or if your baby is stuck in an awkward position. To do a ventouse delivery you need to have adequate pain relief, the cervix needs to be fully dilated, move the baby’s head must move down when you push, and there needs to be enough space in the pelvis, all of which I assess on vaginal examination, sometimes with the assistance of ultrasound.
It is important for you to know that successful delivery with a vacuum is not always guaranteed. If I think there is a low likelihood of delivery then I might recommend forceps delivery, a caesarean section, or a trial of vacuum delivery in the Operating Theatres, with the option of proceeding to caesarean section if we are not successful. When the vacuum is applied there is a maximum amount of time when the vacuum can safely stay on for, and there needs to be some degree of progress with each pull, whether it is rotation or descent of the head.
If the head does not move at all with the vacuum then I will generally need to do a caesarean section, if there is some descent with each pull then I will generally do up to three pulls to bring the head to the perineum, and up to three pulls on the perineum to deliver the head, and then stop unless the head is
partly out or imminently deliverable.
It is generally safer for your baby if I use just one instrument, so if I do not think that vacuum is likely to be successful I will recommend forceps. This is likely to be the case if the head is not very low in the pelvis, if there is a lot of swelling on the back of the baby’s head (known as caput), so the suction cap is likely to fall off, or if the baby’s head does not move with pushing. If I do not think either ventouse or forceps can be attempted safely I will recommend caesarean section.
Following ventouse delivery your baby will have a small round “bun” on the back of their head, known as a “chignon”, in addition to the swelling that occurs naturally from being upside down in the pelvis. This usually settles within a few days. There is often a dark purple disc which can persist for around ten days. Sometimes the skin on the scalp is lifted slightly, or there is soft swelling under the scalp, known as cephalhaematoma, which generally settles down after a few days. Occasionally this causes the baby some irritation, and your Paediatrician may prescribe baby Panadol.
Serious complications as a result of ventouse delivery are rare, especially if we limit the number of pulls and the amount of pressure applied. One of the rare but serious complications of ventouse delivery is known as a sub-galeal tear, which is when the scalp is lifted from the skull, forming a large blood clot or bruise underneath. Sub-galeal tears occur once in every 200 ventouse deliveries, and can be minor, in which they are of no consequence, or major, in which case your baby will need to be transferred to the neonatal nursery for intravenous fluids and monitoring. Another rare complication is skull fracture.
Perineal Repair:
If you have a cut or a tear then I will suture or stitch the perineum with a dissolving stitch. This is usually a suture material known as Vicryl. In the deep layers the Vicryl is slowly dissolving, and takes two to three months to dissolve. In the skin layer the Vicryl dissolves after two or three weeks.
Because of the proximity of the perineum to the anus, and the multiple bacteria that live in the area it is very easy for the perineum to become infected. For that reason I cleanse the perineum extensively, before, after the repair, and I advise you to keep the perineum as clean and dry as you can after the birth. You sometimes need antibiotics to prevent or treat perineal infection. Antibiotics are safe for the baby, but I recommend a probiotic, such as Qiara, if you need antibiotics around the time of birth.
If there are signs of infection it is important to start antibiotics to prevent breakdown of the perineal repair. Early signs of infection are worsening pain, increasing tenderness, an offensive smell, and increasing redness of the perineum. Starting antibiotics promptly will generally prevent the perineum from becoming truly infected and the wound breaking down. If it does break down it will still heal, but healing will take longer.
Two issues I would like you to consider are for just after the baby is born. The first is the Syntocinon injection that we give you very soon after the birth. It is often said that it is given to speed up the delivery of the placenta but that misses the real point of the injection, which is to reduce your risk of excessive bleeding after the birth. Having the injection halves your risk of post partum haemorrhage. Your blood is precious. Having spent much of your pregnancy trying to maintain good blood and iron stores it makes good sense to have the injection. The second is the Vitamin K injection. This injection helps prevent a rare but potentially serious bleeding disorder, that can cause bleeding in your baby’s brain.
Feeding and Settling:
For many first-time mothers feeding and settling can be a challenge. Most babies do not naturally attach to the breast, they often attach to the nipple. If that is not corrected quickly then it will cause nipple damage, which can be very painful, and take a while to heal. It is important, therefore, for both you and the baby to learn good technique from the outset. Silverette nipple caps can be a great help.
Please take advantage of the expertise and support offered by the midwives on the ward. If necessary, you can be referred to a Lactation Consultant. There are daily drop-in classes, lactation consultant sessions and one-on-one sessions during the week, and sometimes even at weekends, depending which hospital you are booked at.
Your milk generally comes in on day three or day four, but can take up to one week, and occasionally even longer. When it comes in you may be quite tearful. Most babies lose between 5 and 10% of their birth weight in the first few days. If your baby loses much more than 10%, then you may need to supplement the breast milk with some formula, especially if your baby is jaundiced, or low birth weight to start with. This is something that you will be given advice on by your Paediatrician, in conjunction with the Midwife or Lactation Consultant.
When you go home remember to send a text to my midwife, Michele (or Chantelle), who will arrange to do a telehealth home visit, to make sure that the feeding and settling is going well. This is a very important service, and one that I am very proud of, so please take advantage of it. If Michele identifies a need for on-going support she will advise how to go about that, and, if necessary, help to put it in place.
Sleep:
By far the most difficult challenge facing new mums is coping with sleep deprivation. Before the birth please take some time to consider how you personally will cope with sleep deprivation. Most new mums are not prepared for just how difficult it can be to adjust to having a newborn, who, while delightful and engaging in every other way, wants to stay awake all night, and feed, cry, or play, or all of the above.
Most babies will sleep in patches during the day, so please take advantage of every opportunity during daylight hours when your baby sleeps to have a rest yourself as well. If partners or family are around, then they can often take the baby for walks during the day, while you rest, so put them to work.
I recommend limiting visitors to close family. Visitors are well meaning, but often draining at a time when you need all your energy and resources, and above all, sleep. Take advantage of every offer of help from practical things such as shopping, cooking and cleaning, and offload peripheral responsibilities. Since COVID-19 the night nursery at POWPH has been closed.
The good news is that there is light at the end of the tunnel. For a while you may feel like there is a heavy fog hanging over you, preventing you from functioning normally and making rational decisions. Over time you usually become more accustomed to broken sleep, and you will learn to take advantage of whatever sleep opportunities you have.
Above all else I think it is important not to torture yourself trying to do things perfectly. Most first-time mums especially want to do everything perfectly, and if it works then that is fantastic, but please have a plan B. Sometimes you will need to give your baby formula top ups and that is perfectly OK, even if it is not your first preference. Sometimes formula top ups are necessary for a variety of reasons, and your baby will still be strong and healthy and still love you just the same.
Please remember to collect your copy of Dr Howard Chilton’s book, “Baby on Board”. I may give you a script for pain medications, if you are likely to need them after discharge from hospital, especially at RHW. The POWPH pharmacy dispenses any discharge medication you need.
I look forward to finishing this journey, and remember, it will all be worthwhile when you are holding the
little one in your arms.
Labour
Labour can start gradually or all at once. You may experience some “practice” contractions before true labour starts. Contractions become more frequent and more intense as labour establishes.
You will often make better progress in labour in your home environment, however if you need pain relief or feel you may be progressing rapidly then you should ring the Delivery Suite and come into hospital. When you are having regular, painful contractions that are five minutes apart, or your waters have broken, it is time to contact the Delivery Suite at your booked hospital.
Please ring the Delivery Suite at your hospital before you leave and remember to bring your antenatal card. If you are unsure whether you should go to the hospital please ring the Delivery Suite and a midwife will give you phone advice. If you feel you really need to come in please do come in.
On arrival at the Delivery Suite a midwife will assess you and your baby and then notify me of your admission and progress. During your labour you and your baby will be assessed regularly. If the labour is progressing well you may not see me until close to the delivery time, however I shall be in close telephone contact with the midwife looking after you, and readily available should I be needed.
If you are having a planned caesarean section and you start to go into labour or your waters break before the planned date, please notify the Delivery Suite immediately. There is no need to panic, but you will need to come into hospital immediately for assessment. Please do not have anything to eat or drink, in case your caesarean needs to be performed quickly.
Pain Relief After Birth
Pain Relief Principles
Most pain killers have side effects for the mother and cross the placenta (during pregnancy) and into breast milk (when breast feeding), but in very small doses in both cases. You can expect discomfort after birth, but you should not be in severe pain. If you need pain relief medication you should take the lowest dose of the safest medication to keep you comfortable, and to prevent severe pain.
On discharge from hospital I recommend the following for pain relief, if required:
Paracetamol (Panadol):
Panadol is quite mild on its own but is much more effective when taken regularly, and greatly reduces the amount of stronger pain killers you need, so it should be your baseline pain killer, and the last one to stop.
Non-Steroidal Anti-Inflammatories NSAID (eg Voltaren/Meloxicam):
Anti-inflammatory medications are usually stronger than Panadol. They help with both pain and swelling. They are excellent for stitch pain, "after pains" and caesarean scar pain. They can cause gastric upset, even ulcers, and can increase blood pressure, so must be used with care if you have high blood pressure, pre-eclampsia, or gastric ulcers.
Opioids (eg Endone/Tramadol/Palexia):
Opioids are very strong pain killers derived from Morphine. They are excellent for severe pain, eg after caesarean. They can cause sedation, constipation, dizziness, drowsiness and even hallucinations. They are addictive and should be used short term only for breakthrough pain in addition to Panadol and an NSAID, and stopped as soon as possible.
NB. If you have had a caesarean section you should avoid driving for 3-4 weeks and avoid heavy lifting (more than 10kg) for three months.
Midwife Support:
Bridget Flannery
Tel: 0417 821 438
You will have one or two antenatal telehealth sessions with Bridget, to help cover midwifery aspects of your preparation for birth and to be a parent, including feeding. You will have a postnatal consultation with Bridget to provide practical advice, help and reassurance after you have had your baby. The main focus is on postnatal recovery, breastfeeding and settling advice, and to discuss any difficulties you may be experiencing as new parents. I offer face to face midwife consultations in my Edgecliff rooms and I am looking to reintroduce home visits for your postnatal check in 2025 if you are local.
You can communicate with Bridget by phone or text message, preferably between the hours of 8am and 9pm most days. Please note that Bridget has a busy hospital schedule, and also has a family, so reason she may not be contactable on some days, overnight or some weekends. The cost of the care and advice that Bridget provides, including one home visit, is incorporated in your planning and management of pregnancy fee.
Bridget is not able to provide an emergency service. In an emergency please contact the Delivery Suite of the hospital at which you are booked.
I have emergency spots available most days in my rooms.
Preparing for Labour and Birth
Birth usually occurs between 39 and 41 weeks of pregnancy. Here are a few suggestions to prepare:
Mind Preparation
Connecting your mind with your baby may help both the baby and your body to release the hormones that will initiate labour. Talking to your baby, being aware of baby’s movements and imagining what life with your baby will be like as you go through your day to day activities eg: shopping, driving, may help you to connect and prepare you better for the reality of being a mum. Yoga, relaxation, hypnobirthing sessions, meditation, visualization and prenatal classes may also help.
Body Preparation
Helping your baby to adopt a head-down, anterior (back facing the front) position will optimize your chances of having a normal labour and birth. Leaning forward over the kitchen bench and rocking your pelvis for a few minutes several times each day in the last few weeks of pregnancy may help. Avoid leaning back in lounge chairs, instead adopting a leaning forward position when sitting may also help. Remember not to sleep on your back as it may decrease the blood flow that you and your baby receive. It is best to lie go to sleep on your left side, and not flat on your back.
Acupuncture
It is recommended to start acupuncture for birth preparation from week 37. Acupuncture at this time is designed to help you achieve the best balance possible – improving energy levels, finding a sense of calm, whilst working to optimise positioning of baby, ripen the cervix. We help get your body and mind as ready as possible for this incredible life transition. Consider Eastern Therapies or Red Tent.
Perineal Massage
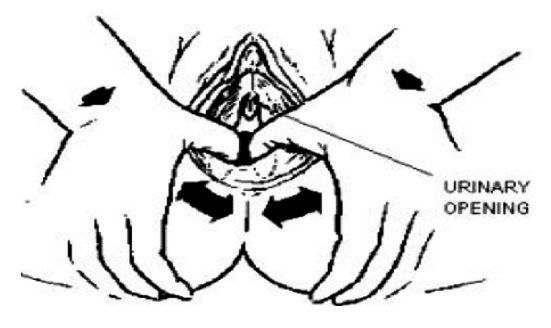
Perineal massage has been used in different countries and cultures throughout much of human history. It is a method of preparing the outlet of the birth passage, particularly the perineum, for the stretchinga nd pressure sensations during the birth of your baby.
The aim is to avoid trauma to that area – either a tear or an episiotomy (a cut made in the perineum to enlarge the outlet). It has been shown that women experiencing their first vaginal birth, who practise perineal massage from 34 weeks onwards, have a lower risk of serious tearing or episiotomy.
Massage can be done internally or externally before your baby is born by you or your partner depending on how comfortable you both are with the procedure. To aid relaxation prior to the massage, a warm bath or warm small towels placed on the perineum before starting the massage can help to relax the area. A low-irritant oil or cream e.g. vitamin E, or olive oil can be used as a lubricant if desired. Perineal massage can be performed from 34 weeks onward, just 3 times per week for about 5-8 minutes per day. You will notice that the stretchiness and flexibility of your perineum will increase.
First wash your hands, then obtain a mirror and prop yourself up with pillows. Look at your perineum with the aid of the mirror and become familiar with the whole area involved. If you use a lubricant, put it on your thumbs and place your thumbs three to four centimetres inside your vagina and press the inside of the perineum toward the rectum and to the sides. You will feel a slight tingling or burning as you gently press down and stretch the opening.
Maintain this stretching and pressure for about one minute. The area will become a little numb. Work the lubricant in, slowly and gently, maintaining the pressure and pulling the perineum forward a little; this is what your baby's head will do as it is being born. The massage can be in one direction at a time i.e. from side to side, or the fingers can be swept in the opposite direction. Try different ways until you find which is more comfortable for you. This massage should not be painful.
If your partner does this massage, the perineum and sides are pressed by using his two index fingers. He massages with his index fingers inside and his thumbs outside. This is a very intimate and private area and sensitivity within the relationship with your partner is essential.
Perineal massage will make you more aware of this area and will assist you to relax and open up for your baby's birth. During the bearing down stage of labour it is common to tense and try to hold back. Women who have consistently done perineal massage do not report the extremes of stinging and burning that often accompany the birth of the baby's head. It is hoped that because the stinging and uncomfortable burning sensations are reduced, you will be able to relax more and allow your baby's head to slip over an intact perineum. Be prepared to have a slow, controlled birthing of your baby's head. Pant/blow to overcome pushing sensations as the head emerges.
Pelvic floor exercises should be practised daily throughout pregnancy. This practice will help you to be able to consciously relax the muscles of the pelvic floor, which is exactly what you will do to assist in the birth of your baby. Perineal massage prior to crowning may help reduced perineal tearing. Pelvic floor exercises after birth will help you to re-tone your stretched muscles and tissues.
Please note:
• You can massage over previous episiotomy scars.
• It is advisable not to use perineal massage if you have any lesions or active herpes during this stage of pregnancy
Epi-No
The Epi-No device is a device for perineal stretching. It is a relatively new invention (15 years) and the evidence supporting its use is still somewhat conflicting. It may, however, reduce the likelihood of having a major perineal tear. It costs around $280, and can be purchased from the hospital Foyer Pharmacy, and can be used as an alternative or in addition to perineal massage, from 36 weeks.
Ripening of the Cervix (things to do if you are 37 weeks or more)
Nipple Stimulation:
Oxytocin, a hormone that initiates labour, is released when nipples are stimulated and breasts are expressed. Roll one nipple at a time between finger and thumb alternating positions of fingers as breasts may be tender. You may want to express your breasts (squeeze breasts in a pumping action for 10 minutes at a time as often as you like at least 3 times per day (ask us to show you how). You may notice some colostrum (milk) coming out. In many cases, expressing at the end of pregnancy can increase the amount of breast milk you will have for your baby (only to be done after 36 weeks).
Membrane sweeping & stretching:
This should only be done by a midwife or doctor and involves a vaginal examination, stretching of the cervix, and separation of the membranes from the cervix. It is generally very safe, when there are no complications. Often the procedure can cause discomfort and bleeding (a “show”) and sometimes, irregular contractions. It may however help you to go into spontaneous labour earlier than otherwise.
Acupuncture:
Regular acupuncture sessions have been shown to decrease stress and increase energy levels, helping you to cope with the final weeks of pregnancy and labour. Some studies suggest it may assist with the initiation of labour, although the evidence is not strong, just like with eating dates.
Acupressure: (Only to be used after 37 weeks to help initiate labour)
Stimulating points on the feet and hands can stimulate other parts of your body ie: uterus and help labour hormones to be released. Locate the points illustrated in the pictures below, ie SP6 is 4 fingers up from the top of the ankle bone. The points may be tender when you press them. Press firmly with your thumb for about 5 minutes each 1-2 hours. It’s normal that your baby may move during acupressure. Feeling hot, flushed, teary or experiencing a contraction during the point stimulation is also normal, and will show that the treatment is effective. See https://acupuncture.rhizome.net.nz
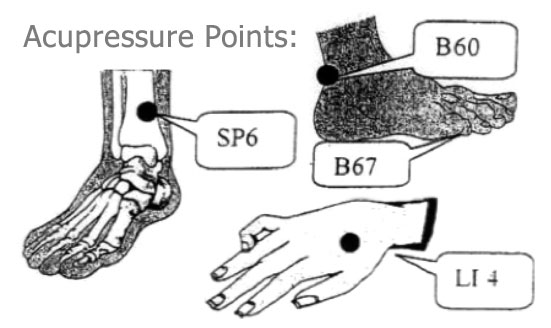
Intercourse:
Semen contains prostaglandins, which are hormone-like substances that help soften the cervix, so it may start to dilate. The cervix responds to intercourse only at the end of your pregnancy, and it is generally safe to have sex throughout your pregnancy, unless you have been advised not to. It is common for many women to find it uncomfortable toward the end of pregnancy, so trying the above alternatives instead may be just as beneficial in terms of preparing for labour.
When to Contact the Hospital
It is very important that you ring the Delivery Suite before leaving home. The Midwife will ask you some questions about your labour and answer any questions you may have.
Contact Numbers:
Delivery Suite, Prince of Wales Private Hospital
Tel: 9650 4444
Delivery Suite, Royal Hospital for Women
Tel: 0439 869 035 or 9382 6100
Women expecting their first baby
If you are close to your due date (37 weeks or more), we recommend that you come to hospital:
• When you are having regular labour pains, which are becoming stronger, closer together and are
lasting 60 seconds, from the beginning to end. At this time most women will find the labour pains
are about 3 to 4 minutes apart (from start of one contraction to the start of the next);
Or
• When your ‘waters break’- this is when the bag of waters around the baby breaks. It might be a
slight trickle or a sudden gush followed by a constant flow of fluid. When this happens it is a good
idea to put a pad on, so we can check the colour/odour of the fluid when you arrive
Or
• If you have any bright bleeding, that is heavier than a normal ‘show’ (blood-stained mucus)
If you are less than 37 weeks we advise that you come to the hospital as soon as you have any signs
of labour, i.e. labour pains, broken waters, vaginal bleeding or ‘show’.
Women expecting their first baby
All of the above applies except that you are advised to come to hospital when your contractions are
regular, painful and about 5-7 minutes apart.
Other reasons to call the hospital at any time during your pregnancy
• If you have a constant, strong, abdominal pain, lasting more than 60 minutes
• If you notice a reduction in your baby’s movements ie: your baby is moving less than usual, or there is not a “window” of two hours each day, during which your baby moves at least ten times
• If you have symptoms of high blood pressure ie: headaches, visual disturbances or tummy pain
• If you have a constant itch all over your body, particularly on your hands and feet
• If you have heavy, fresh, vaginal bleeding
Birth Photography
If you are looking for a great photographer with a special interest in birth I recommend Shirin Town.
eMail: shirin@shirintown.com
Tel: 0404 063 441
What To Bring To The Hospital
Below is a list of suggestions of what to bring to hospital for the birth of your baby.
For the car – put this in the car after 24 weeks
• 2 clean old towels plus pads, spare underpants and black ankle length tights to change into if your waters break
• Plastic container with a lid (in case of vomiting)
• Please ensure you have an approved, fitted car restraint for your baby in your car prior to labour
For Labour and Birth
• Wear whatever you feel most comfortable in for labour and birth, ideally a large comfortable T–shirt, sarong & socks to keep feet warm. The birth suites offer a hospital gown if you prefer.
• Toiletries - soap, toothbrush, toothpaste, deodorant, shampoo, brush, comb, face cloth, hair tie.
• Tissues
• Vaseline or lip balm
• Lollies or lollipops to suck
• Music
• Aromatherapy oils – massage oil – vapourisers are available if you want,
• TENS machine
For partners or support people
• Snacks and. Water bottle. Tea and coffee making facilities are available
• Loose comfortable clothing and a jumper as the hospital is air-conditioned
• Change of clothes/toiletries, razor etc (you may be there a long time!)
• A pen and paper can be useful
• Swimmers/board shorts (you might get wet if your partner is using bath /shower in labour!)
• Camera,
• Phone & camera charger
• Nice, comfy pillow from home
For your post-natal stay
Pack these in a separate bag or in the bottom of your case.
• Comfortable casual clothes for day wear, nightwear, dressing gown and slippers. Front opening
nightwear or loose T-shirts are more convenient for breastfeeding
• 3-4 maternity bras/loose Maternity singlets to allow for breast growth
• Breast pads
• 3 packs of maternity sanitary pads (with wings) and comfortable, sensible underpants
• Toiletries and hairdryer
• Pen and paper
• Phone & camera charger
For baby
• Disposable nappies (if attending RHW, otherwise supplied at private hospital)
• If you are planning to formula feed your baby, you will need to bring your own bottles & formula
• An outfit and a blanket or wrap for taking your baby home (bring a spare in case of accidents).
Please remember to bring your antenatal card
Parking reminder: when you come in to either hospital to have your baby please remember to buy a 5 day car park pass, as this can reduce your parking costs somewhat.
Suggested List of Items for your Newborn
Items must comply with Australian Safety Standards. For further information ring Standards Australia 1300 308 989 or visit their website www.standards.org.au
| Cot (bassinet optional) travel cot (optional) | Pram/stroller (with rain cove) |
| Towels / face cloths | Breast Pump (double electric are best) |
| Firm, well fitted mattress and mattress protectors (2) | Baby carrier (ensure it has good head support for baby and back support for you) |
| Cloth nappies x 24 (fasteners safety pins, “snappy nappy clips”, pilchers, nappy bucket, nappy liners). A “nappy service” may be a great option. | Car restraint (capsule/ seat) you can hire a car capsule for the first 3 months apparently it’s safer than a 0-4 car seat. |
| Large scarf/sarong /wrap to cover breasts whilst feeding and pram whilst baby is sleeping. | Sunshades for car and mirror for back window so you can see your baby facing rearwards |
| Cotton or woollen blankets (no doonas) | Baby Panadol |
| Cot sheets (3): 1 on, 1 in wash and 1 ready to go! | A large handbag to carry spare nappies and baby essentials |
| Jumpsuits /bondsuits x 7 buy a few 0000’s and mainly 000’s | Barrier cream for nappy rash ie zinc and castor oil or petroleum-free paw-paw |
| Singlets / singlet bodysuits x 7 | Newborn disposable nappies |
| Sunhat / beanie | Wraps (7) |
| Socks | Thermometer |
| Cotton wool balls, container for water / Unscented baby wipes | Baby monitor (optional) - must be placed at least a metre away from baby (emits EMR) |
| Change table with mattress, sides, drawers/shelves | Cotton buds to clean belly button |
| Baby bath (with plug/stand: optional) | Sterilizer (optional) |
Silverettes: silver nursing caps: the new way to promote soothing and healing of nursing nipples
NB Hydro-gel pads or "Lansinoh" cream are both controversial, as some sudies have shown an association with mastitis.
What is a Doula?
A doula can provide support and education during your pregnancy and labour, both at home and in the hospital if you need it. They also provide support and advice in the early days and weeks following your birth. Doula fees can vary substantially. You can ask Dr Sen or the Bridget for recommendations.
To find a doula see www.findadoula.com.au or www.australiandoulacollege.com.au
Important: Warning about Cytomegalovirus (CMV)
CMV is a very common virus that many children and adults carry at some stage. CMV can cause a severe flu-like illness, but sometimes no symptoms, and can cause harm to your baby in pregnancy.
CMV is often found in the saliva of infants. It can be transmitted by sharing dummies, food utensils and food with infants, or handling clothes or toys with infected saliva, urine or other bodily fluids or kissing on lips. CMV can be a very serious problem if it occurs just before conception or in early pregnancy.
To avoid transmission of CMV take the following precautions:
• Wash hands often with soap and running water for at least 15 seconds and dry them thoroughly. This should be done especially after close contact with young children, changing nappies, blowing noses, feeding a young child, and handling children’s toys, dummies/soothers.
• Do not share food, drinks, eating utensils or toothbrushes with young children.
• Avoid kissing children on the lips
• Use simple detergent and water to clean toys, countertops and other surfaces that come into contact with children’s urine, mucus or saliva.
Timing of Birth
It is sometimes better for you (and your baby) if your labour starts spontaneously, however if this does
not occur then I would normally plan to induce your labour within one week of your due date, sometimes earlier. The reason for inducing labour, and for most interventions regarding timing of birth, is to minimise the risk of stillbirth. Reassuringly the risk of this is extremely low. The landmark ARRIVE trial reassures us it is safe to induce labour from 39 weeks without increasing the risk of caesarean.
Women with complications in pregnancy, such as high blood pressure or diabetes, may need to be induced earlier. The main disadvantage of inducing labour is that it can make your labour more intense. If we are planning delivery by elective caesarean section I will generally perform this between 39 and 40 weeks, as this time has been shown to be safest for your baby.
Pain Relief
Not all women want or need pain relief in labour. During labour your body naturally produces Adrenaline and Endorphins, natural forms of Morphine, that allow you to cope with labour pains. Also many women find it very comforting in labour to be under the shower, or immersed in a bath of warm water. Other things that can help are massage, a TENS machine and nitrous oxide gas.
If you do want stronger pain relief then there is a range of options available to you, including injections of Morphine or an epidural anaesthetic. If you want or need an epidural you can have one, and it does not need to be booked in advance, unless you want a specific anaesthetist. There is a consultant anaesthetist on call 24 hours a day in both hospitals. Both hospitals use low dose epidural anaesthetic in labour, which provides good pain relief with some degree of mobility.
Perineum and Pelvic Floor
The perineum is the area between the anus and the vagina. The pelvic floor is a sling of tissue, mainly muscle, that supports and controls your bladder and bowel function, and through which your baby passes when coming through the birth canal. I discuss pelvic floor management at your first visit and teach you how to perform a pelvic floor squeeze correctly if necessary. Once you have learned how to do a pelvic squeeze correctly I recommend that you practise regularly during the pregnancy and post-natally, to reduce the risk of bladder leakage and prolapse in later life.
At the birth one of my priorities is to protect your perineum from avoidable tearing. I do not routinely do an episiotomy (cut with scissors), and a small tear is generally better than a cut, however major tears can leave you with lasting pain and problems with lack of bowel control, so there are times when an episiotomy is better. That is particularly the case when forceps or vacuum is required for delivery. You may reduce the risk of tearing by doing perineal massage or by using the Epi-No device.
Cutting the Cord
I usually encourage your partner to cut the cord after I have clamped it. Traditionally the cord was clamped and cut immediately after the birth, however now we usually do delayed cord clamping. Delayed clamping allows more cord blood to flow to the baby and is thought to be especially beneficial for pre-term babies (under 37 weeks).
For babies 37 weeks and older the benefit of delayed cord clamping is less clear – it does give them a higher blood count, but it also gives them higher rates of jaundice, requiring phototherapy, and may result in the baby being separated from you for admission to the special care nursery for treatment.
I usually compromise and cut the cord at around 1-2 minutes. This still gives the baby a little extra cord blood, but does not appear to be associated with higher levels of jaundice, and still allows me to collect the cord blood, either for donation or for private storage.
About Vitamin K
Vitamin K is a vitamin that naturally occurs in our bodies, which helps to clot the blood. After a baby is born it takes weeks to months for their liver to make enough Vitamin K to ensure their blood can clot properly. By giving your baby Vitamin K it makes sure they will have enough to clot their blood and can prevent a rare disorder, known as, haemorrhagic disease of the newborn (HDN). HDN can cause bleeding into the brain and could result in brain damage or, in extreme cases, even death.
Vitamin K can be given to your baby by injection or orally. Only one injection is required, however, oral dosage is more complicated. To give your baby Vitamin K orally you will need to make sure your baby has one dose at birth, one dose between three and five days after birth and another one in their fourth week of life. There are a few reasons babies may not be able to have Vitamin K orally, including if they are ill, if they are born prematurely or if during your pregnancy you have had medication for epilepsy, blood clots or tuberculosis.
One Vitamin K injection is enough to last your baby for months. Vitamin K has been used in Australia for more than 25 years without any apparent side effects and has eradicated HDN. There was one study that suggested there could be a link between Vitamin K and childhood cancer, but this study has since been discredited.
It is your choice whether or not your baby is given Vitamin K. However, medical experts in Australia agree that babies should be given Vitamin K to prevent the very serious disease of HDN. Your baby will be given a Vitamin K within an hour or two after birth. If you would prefer your baby to have Vitamin K orally, please speak to me, and let your midwife know at the birth.
Maternity bras: Getting it right
Your breasts will grow throughout the pregnancy but mostly in the first 26 weeks and in the last few weeks of your pregnancy. It’s normal for your breasts to increase by at least a cup size so it is important to wear a comfortable (non maternity) bra at this time, sports bras may be an appropriate choice.
Underwire bras are not recommended as they can sometimes make your breasts feel uncomfortable and affect the way the milk ducts form. It is a good idea to get a proper feeding bra fitted professionally at around 36 weeks, Your pregnancy bra should generally be bigger than normal, to allow room for breast growth, which will occur after your baby’s birth. Having a few inexpensive breastfeeding crop tops or singlets on hand may get you through the first few weeks after baby’s birth. Many women have an oversupply of breast milk that may last up to 6 weeks. Your breasts will then decrease in size yet still containing enough milk for your baby. Your breasts should generally remain that size for the duration of your breastfeeding time. 6-8 weeks postnatally may also be a good time to have a bra professionally fitted, particularly if you are getting upper back or neck pain.
Probiotics
There is increasing evidence that the use of probiotics may help both you and the baby. Benefits for you include reduced a risk of mastitis and improved bowel health, especially if you need antibiotics. There may also benefits for your baby, especially if he or she is born early or if you need antibiotics.
The most promising probiotics for pregnant and breastfeeding women appear to be either Qiara, Biogaia or Bioceuticals. There is a new probiotic, Infloran, that may be helpful for the babies of women having caesarean section.
Post-Natal Care
I shall visit you regularly in hospital after the birth until you go home. On average you stay 3-4 nights following a vaginal birth and 4-5 nights following a caesarean section.
I want to ensure you have adequate pain relief during your recovery. Usually I prescribe pain medication to be brought to you by midwives on request, but I want to make sure your individual needs are met. I also want you to be able to move about freely, even if that means extra pain medication. If you have had a caesarean section you will have a Prolene (non-dissolving) suture, tied in a loop in front of the scar, that must to be removed by the midwife before you go home.
It is normal to experience swelling of the feet after the birth, even if there was none during the pregnancy. This will settle on its own, usually within 1-2 weeks. Your bowels will usually not open for 2-3 days after the birth. Drinking plenty of water and eating fibre, such as pears and prunes, will help. You may need Movicol or Coloxyl to help prevent you from needing to strain at stool.
The maternity unit at Prince of Wales Private Hospital has recently been refurbished and expanded. The Little Luxuries programme at the Crowne Plaza ceased some time ago. It is unlikely to re-open.
If you are booked at the Royal Hospital for Women, you have the option of early discharge on the Midwifery Support Programme (MSP). Under this programme if you leave the hospital within 48 hours of a vaginal birth or within 72 hours of a caesarean birth the hospital post-natal midwife team will follow you up with visits to your home. If you live out of the area then a cross-referral needs to be made to your local maternity MSP midwifery team, of they have capacity. MSP is limited during COVID-19.
You will have a final telehealth check-up 6-8 weeks after the birth. At this visit I check that everything is back to normal, and any stitches have healed properly. I will also discuss your contraceptive needs.
Length of stay
• If you have a vaginal birth, you can expect to be discharged after 3-4 nights.
• If you have a caesarean you can expect to be discharged after 4-5 nights.
The hospitals do not accept any responsibility for the loss of valuables, credit cards or money whilst in the hospital. It is better not to bring these with you. Please ensure that you have someone available to take you home from hospital. Time of discharge is generally around 10 am for both hospitals
Lower Back, Hip and Perineal Support
Many women experience lower back and hip pain during pregnancy. In addition to physiotherapy, you may well benefit from additional support wear. If you have private health insurance your health fund may provide a rebate for some of the costs of special support wear. Chiropractic, osteopathy or massage may also help. The following sites provide to supportive clothing that may be of help:
SRC recovery shorts: http://www.recoveryshorts.com/
Wraps and support belts: http://www.duesoon.com.au/
These may best be fitted after consultation with a physio, chiro or osteopath. You may be eligible for a
health fund rebate.
If you are experiencing great difficulty in finding a position in which you can sleep comfortably, you may
like to look into the Belly Bed – Tel: 1300 961 110 or www.thebellybed.com.au
Administration and Planning
Hospital Bookings
I deliver babies at the Royal Hospital for Women and the Prince of Wales Private Hospital, Randwick. Prince of Wales Private Hospital is my preferred hospital
Practice Locations
Edgecliff Practice: located at Suite 502, Level 5, Eastpoint Tower, 180 Ocean Street, Edgecliff, on the corner of New South Head Road. There is free 2-hour parking at Eastpoint Food Fair Car Park on New McLean St (not the Aldi car park).
Drive past the Aldi car park to the Eastpoint Food Fair car park and park on level 2 (Yellow). Take the far “Resident” lifts to level 5. Alternatively, from Edgecliff Station or Eastpoint Food Fair, take the stairs or resident lifts between the butcher and Coles.
City: Suite 704, Level 7, BMA House, 135 Macquarie Street, Sydney on Thursday mornings. Parking in the CBD is limited, but the rooms are only a short walk from Martin Place and Circular Quay, and only 10-15 minutes by train from Edgecliff.
Surgery Hours
Monday-Thursday 9.20am-5pm.
On Fridays I have my operating list at Prince of Wales Private Hospital
To book an appointment call 02 9363 9474 or email: admin@rahulsen.com.au
After Hours and Holiday Cover
I am on call for you 24 hours a day during the week and I always strive to be present for the birth of your baby. However, it is not possible to be on call all day every day of the year! No obstetrician can give a 100% guarantee of being present at the birth, although last year I attended 99% of births. I generally take one weekend or one long weekend off per month.
If I plan to be on leave I will arrange cover with another specialist obstetrician, either Dr Bobby Teoh, Dr Stephen Coogan, Dr Wendy Hawke, or Dr Jason Chow who will take excellent care of you. Dr Sarah Lyons has also joined our group, and is currently on maternity leave.
I try to book holidays well in advance, so that I can notify you of planned leave during your pregnancy. I take 4-6 weeks annual leave each year. In 2025 I have planned leave from 6 February to 1 March, 24 July to 15 August and 18 December to 8 January. I also take time to attend courses and conferences that keep me up-to-date with all the latest developments and evidence-based best practice.
I have at least one emergency slot available every day in case you need to be seen urgently, so please ring my rooms to make an appointment.
I understand that your partner and family members are concerned for your welfare and may want to talk to me, but I only discuss your condition or results with you. Please note that I do not conduct consultations or discuss results by telephone.
If you experience constant, severe pain, bleeding, reduced fetal movements or signs of labour then
please ring the delivery suite of the hospital at which you are booked.
Fees
It is a Government requirement that you receive informed financial consent. You should have received a schedule of my fees and an acceptance form for you to sign and bring back.
When you are admitted to hospital most of your fees, including tests and medications, may be covered by your health fund, depending on what type of cover you have. Please check these costs with your fund prior to booking into the hospital. Please also check that your baby will be covered in the event of an admission to the neonatal nursery.
Australian health funds do not cover any costs incurred prior to admission to hospital, and do not provide any rebate for the planning and management fee.
Please let me know if you do not have full obstetric cover with an Australian private health insurer or if you are not covered by Medicare, as this will affect your schedule of fees.
Please note that electronic funds transfer is the preferred method of payment of fees. All credit
card payments are subject to a fee of 1.5% to cover bank fees.